Every year, millions of people in the U.S. skip doses or stop taking their meds altogether-not because they don’t need them, but because they can’t afford them. The price tag on a brand-name prescription can be shocking: $300 for a month’s supply of a blood thinner, $200 for a cholesterol pill, $400 for a diabetes drug. Meanwhile, the generic medication version of the same drug costs $4 to $15. That’s not a typo. It’s the reality for most people who switch.
They’re the exact same drug-just cheaper
Let’s clear up the biggest myth right away: generic medications aren’t weaker, older, or lower quality. They contain the exact same active ingredient, in the exact same strength, delivered the exact same way as the brand-name version. If your doctor prescribes Lipitor (atorvastatin), the generic version is chemically identical. The FDA requires this. No exceptions.
The only differences? The color, shape, or packaging. Those are inactive ingredients-fillers, dyes, coatings-that have zero effect on how the drug works in your body. Think of it like buying a plain white T-shirt instead of the same one with a logo. Same fabric, same fit, same comfort. Just cheaper.
The FDA’s approval process for generics is strict. Before a generic hits the shelf, manufacturers must prove it delivers the same amount of medicine into your bloodstream at the same rate as the brand. This is called bioequivalence. The FDA demands that the generic’s absorption rate falls within 80% to 125% of the brand’s-meaning the difference is tiny, clinically meaningless, and tightly controlled.
How much money can you actually save?
Real numbers matter. Here’s what switching to generics saves people right now:
- Warfarin (generic) vs. Coumadin (brand): $4 vs. $300 per month
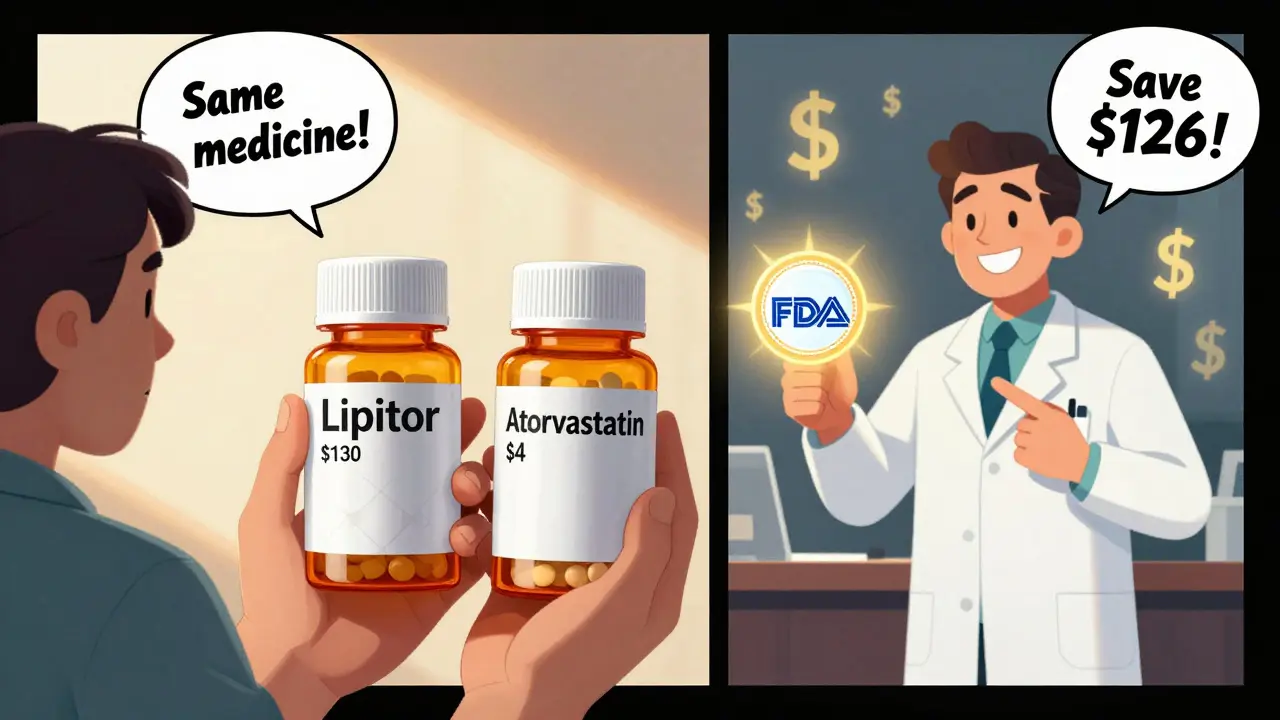
- Atorvastatin (generic) vs. Lipitor: $4 vs. $130 per month
- Fexofenadine (generic) vs. Allegra: $10 vs. $30 per month
- Metformin (generic) vs. Glucophage: $4 vs. $300 per month
These aren’t outliers. They’re standard. According to the FDA, generic drugs cost, on average, 85% less than their brand-name equivalents. And it’s not just individuals saving. In the last decade, generic drugs saved the U.S. healthcare system over $1.6 trillion. That’s money that stays in people’s pockets, keeps insurance premiums lower, and helps public programs like Medicare stretch further.
Insurance plans know this. Most have tiered copay structures: $1-$10 for generics, $25-$75 for brand names. Some plans don’t cover brand-name drugs at all unless you’ve tried and failed the generic first. That’s not a punishment-it’s smart economics.
Are generics as safe and effective?
Yes. And the science backs it up.
A 2022 study in the Journal of Managed Care & Specialty Pharmacy looked at over 100,000 patients taking generic vs. brand-name heart medications. No difference in heart attacks, hospitalizations, or death rates. Another study in the Journal of the American Heart Association tracked 186,000 patients with cardiovascular disease. Same result: generics performed just as well.
Even for complex conditions like epilepsy or thyroid disorders-where people worry about tiny variations in blood levels-the FDA says approved generics meet the same standards. The agency reviews every batch, inspects every factory (over 1,200 inspections a year), and monitors adverse events. In fact, adverse event reports for generics are proportional to their usage-90% of prescriptions are generics, so 90% of reports come from them. That’s not a red flag. That’s normal.
Some doctors still hesitate with narrow therapeutic index (NTI) drugs, like warfarin or levothyroxine, because small changes in blood levels can matter. But even here, the data doesn’t support fear. A 2023 review of over 5,000 patients found no increased risk of complications when switching to generic levothyroxine. The FDA’s position is clear: if it’s approved, it’s safe.
Why do people still hesitate?
Mostly because of appearances.
One patient on Drugs.com wrote: “My pharmacy switched generic manufacturers. The pill changed from blue to white. I panicked. Thought it was a different drug.” That’s understandable. We’re trained to associate pills with brands. But the color change? It’s just dye. The active ingredient? Still identical.
Another common fear: “What if the generic doesn’t work as well?” But when patients actually switch, the results are clear. A 2023 study in Research in Social and Administrative Pharmacy found that people using generics were 68% less likely to skip doses because of cost. That’s huge. Taking your meds regularly matters more than whether the pill is blue or white.
Pharmacists are trained to help with this. When you pick up a new prescription, ask them: “Is there a generic version?” They’ll tell you. They’ll explain it’s the same drug. And if you’re nervous, they can give you a printout from the FDA’s Orange Book-the official list of approved generics and their therapeutic equivalence ratings.
Who’s behind the push for generics?
Not just pharmacies or insurers. Doctors. Hospitals. The government.
The American Medical Association recommends prescribing generics whenever possible-not to cut corners, but to help patients stick to their treatment. Hospitals use generics for 99% of their inpatient meds. Retail pharmacies stock them because they’re cheaper, faster to refill, and less likely to run out.
The FDA doesn’t just approve generics. It actively works to speed up their entry into the market. Their Generic Drug User Fee Amendments (GDUFA) program has cut review times to under 10 months for priority applications. They’re also cracking down on companies that delay generic entry by blocking access to brand-name samples for testing-a tactic called “product hopping.” The CREATES Act of 2019 made that illegal.
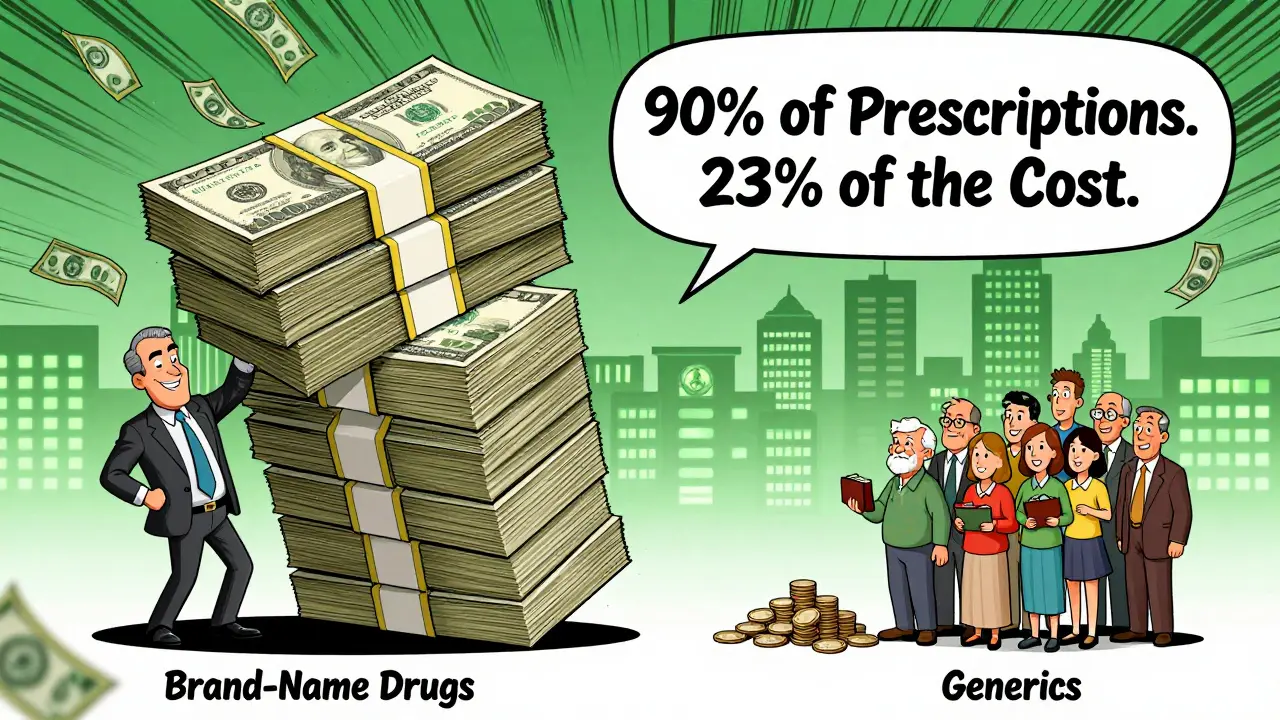
And it’s working. In 2023, generics made up 90.3% of all prescriptions filled in the U.S.-but only 23.1% of total drug spending. That’s the power of competition. When five companies make the same drug, prices drop by 85%.
What about newer drugs? Are generics available?
Yes, but not immediately. Brand-name drugs are protected by patents-usually 20 years from filing. Once the patent expires, other companies can apply to make generics. That’s why you don’t see generics for brand-new drugs like the latest weight-loss pills. But most common medications-blood pressure, cholesterol, diabetes, antidepressants, antibiotics-are already generic.
And the next wave is coming: biosimilars. These are generic versions of complex biologic drugs-like Humira or Enbrel. As of December 2023, the FDA has approved 37 biosimilars. They’re not exact copies (biologics are too complex), but they’re proven to work the same way. They’re already saving patients thousands per year.
How to switch-step by step
Switching is simple. Here’s how:
- Check your prescription. Look at the name. If it’s a brand name (e.g., “Lipitor”), ask your pharmacist: “Is there a generic?”
- Ask your doctor: “Can I switch to the generic version?” Most will say yes. If they’re unsure, ask for the FDA’s Orange Book listing.
- When you get the prescription, confirm the pill looks different. Don’t panic. It’s normal.
- Take it as directed. No adjustment period is needed for most drugs.
- Monitor how you feel. If you notice real changes-new side effects, worsening symptoms-contact your doctor. But don’t assume it’s the generic. It’s more likely stress, diet, or another factor.
Pro tip: Use mail-order pharmacies or discount programs like GoodRx. Even if your insurance doesn’t cover the generic fully, you can often pay under $10 out-of-pocket.
Bottom line: It’s safe, it’s effective, and it saves money
There’s no reason not to switch. Generics aren’t a compromise. They’re the standard. The same medicine, at a fraction of the cost. Millions of people take them every day-without knowing it. And they’re healthier for it.
If you’re paying $200 a month for a brand-name drug, you’re not being loyal to the brand. You’re paying for advertising, research that happened 15 years ago, and corporate profits. The active ingredient? That’s not owned by anyone anymore. It’s public. And you deserve to use it.
Ask your pharmacist. Ask your doctor. Ask your insurance. Switch. Your wallet-and your health-will thank you.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generic medications to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. This means they work the same way in your body. Large studies involving hundreds of thousands of patients have shown no difference in effectiveness for conditions like high blood pressure, cholesterol, diabetes, and depression.
Why do generic pills look different?
The difference in color, shape, or size is due to inactive ingredients like dyes or fillers, which don’t affect how the drug works. These are changed to avoid trademark issues with the brand-name version. The active ingredient-and its effect-is identical. Many patients worry about this, but it’s purely cosmetic.
Can switching to a generic cause side effects?
Rarely. Most side effects come from the active ingredient, which is the same in both versions. If you experience new symptoms after switching, it could be due to a change in inactive ingredients (like a dye you’re sensitive to), but this is uncommon. Always report new side effects to your doctor or pharmacist. The FDA’s adverse event database shows no increased risk of side effects with generics compared to brand-name drugs.
Are all generic drugs approved by the FDA?
Yes. Every generic drug sold in the U.S. must be approved by the FDA through the Abbreviated New Drug Application (ANDA) process. The FDA inspects manufacturing facilities worldwide and requires proof that the generic matches the brand in strength, purity, and performance. If it’s on the shelf in a U.S. pharmacy, it’s FDA-approved.
How do I know if a generic is available for my medication?
Ask your pharmacist or doctor. You can also check the FDA’s Orange Book, which lists all approved generic drugs and their therapeutic equivalence ratings. Most common medications-like metformin, lisinopril, or atorvastatin-have multiple generic options. If your prescription is still branded, it may be because the patent hasn’t expired yet.
Will my insurance cover generics?
Almost always-and at a much lower cost. Most insurance plans have tiered copays, with generics costing $1-$10 per prescription compared to $25-$75 for brand-name drugs. Some plans require you to try the generic first before covering the brand. Using generics helps keep your premiums lower overall.
Is it safe to switch from a brand-name drug to a generic while taking it long-term?
Yes. Millions of patients switch safely every year. For most medications, no adjustment period is needed. The FDA and medical societies confirm that generics are interchangeable with brand-name drugs. If you’re concerned, talk to your doctor before switching. But don’t delay switching because of fear-studies show people who use generics are more likely to take their meds regularly, which improves health outcomes.



Raushan Richardson on 28 December 2025, AT 10:36 AM
Switched my blood pressure med to generic last year and haven’t looked back. Saved $200/month-literally paid for my dog’s annual checkup. Why pay for branding when the science is identical?