The VA formulary isn’t just a list of drugs-it’s the backbone of how millions of veterans get affordable, reliable medication. If you’re a veteran using VA healthcare, understanding this system means knowing exactly what you’ll pay, what’s covered, and how to get the drugs you need without delays or surprises.
What Is the VA National Formulary?
The VA National Formulary is the official list of medications that every VA medical center, clinic, and pharmacy across the U.S. must stock and prescribe. It’s not optional. If a drug is on the formulary, it’s available to you, no matter which VA facility you visit. If it’s not on the list, you’ll need special approval-or a different option. This system started in 1998 and has been refined ever since. Today, it covers over 9 million enrolled veterans through 1,293 VA facilities. The goal? Provide high-quality care at the lowest possible cost. And it works: the VA achieves a 92% generic medication use rate, far higher than the 89% average for private insurers.How the Three-Tier Copay System Works
Your out-of-pocket cost for prescriptions depends on which tier the drug falls into. There are only three tiers, and they’re simple:- Tier 1: Preferred generics. These are the cheapest. Most common medications like aspirin, ibuprofen, atorvastatin, and sertraline fall here. Copay: $0-$5 for a 30-day supply.
- Tier 2: Non-preferred generics or some brand-name drugs with generic alternatives available. Copay: $8-$12.
- Tier 3: Brand-name drugs with no generic version, or specialty medications. Copay: $15-$20.
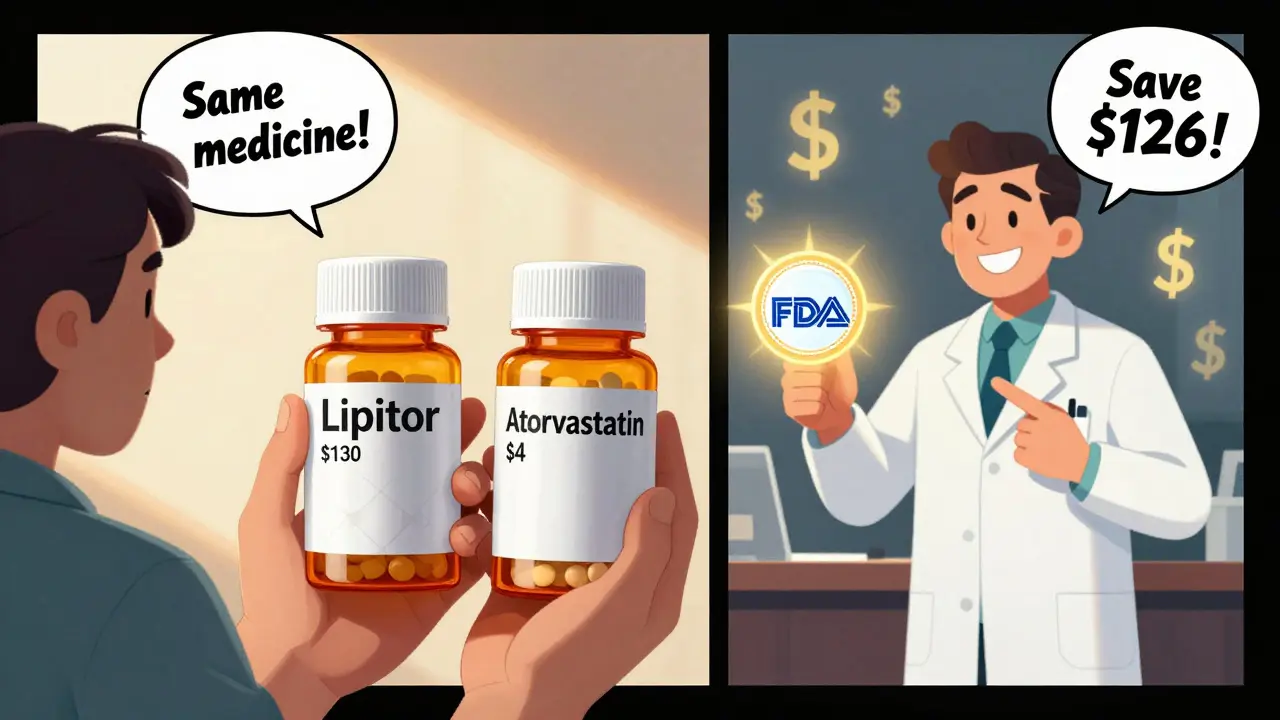
Why Generics Are the Default
The VA doesn’t just prefer generics-it requires them. Unless your provider documents a medical need for a brand-name drug (like a rare allergy or absorption issue), you’ll get the generic version automatically. This isn’t just policy-it’s law-driven efficiency. Generic drugs are identical in active ingredient, dosage, safety, and effectiveness to their brand-name counterparts. The FDA requires them to meet the same strict standards. The VA’s strict generic-first rule saves veterans an average of $15-$40 per prescription compared to commercial pharmacies. In 2024, this approach saved the VA $2.8 billion in pharmaceutical spending. That money stays in the system to help more veterans.What’s Covered in Tier 1? Real Examples
You don’t need to guess what’s in Tier 1. The VA publishes a full list, updated monthly. Here are some common ones you’ll find:- Arthritis & Pain: Allopurinol, ibuprofen, naproxen, acetaminophen
- Cholesterol: Atorvastatin, pravastatin, ezetimibe
- Blood Pressure: Hydrochlorothiazide, furosemide, lisinopril
- Depression & Anxiety: Fluoxetine, sertraline, trazodone
- Diabetes: Metformin, glimepiride
- Thyroid: Levothyroxine

VA vs. Medicare Part D: A Clear Difference
If you’re on both VA benefits and Medicare Part D, you might be confused about which drug plan to use. Here’s the key difference: Medicare Part D often has five tiers. Specialty drugs like GLP-1 weight-loss medications (Wegovy, Ozempic) can land in Tier 5-with copays over $100. The VA? Even if you’re on Wegovy, it’s only covered if you have type 2 diabetes, heart disease, or severe obesity with related conditions. But if you qualify? Your copay is still $5-$15. The VA doesn’t treat weight-loss drugs as luxury prescriptions. It treats them as medical tools. But it also sets strict boundaries. If your doctor wants to prescribe Wegovy for general weight loss (not tied to diabetes or heart risk), you’ll be denied under current CHAMPVA rules effective January 2025.How to Check If Your Drug Is Covered
You don’t need to call someone or wait for an appointment. Use the VA Formulary Advisor tool on VA.gov. Just type in the drug name-generic or brand-and it tells you:- Which tier it’s on
- Whether a generic is available
- If prior authorization is needed
- Alternative options if it’s not covered
Getting Your Meds: VA Pharmacy, Meds by Mail, or Community Care
You have three ways to get your prescriptions:- VA Pharmacy: Pick up at your local VA clinic. Good for urgent needs.
- Meds by Mail: Free, no-copay delivery for maintenance meds. No deductible. Most veterans use this for monthly drugs like blood pressure or antidepressants. 87% of users rate it highly.
- Community Care: If you’re far from a VA facility, you can get prescriptions filled at a local pharmacy-but only if the drug is on the formulary and you have prior approval.
Common Problems and How to Fix Them
Not everything runs smoothly. Here are the top issues veterans face-and how to solve them:- “My doctor wants me on a drug that’s not covered.” Ask for prior authorization. Your provider fills out a form explaining why the generic won’t work. Many approvals happen within 48 hours.
- “I switched to generic and feel different.” 12% of veterans report this. But 94% say they adjust after talking to their VA pharmacist. Don’t stop your meds-call your provider. Sometimes it’s a filler difference, not the active ingredient.
- “I don’t understand my copay.” 35% of new enrollees get confused between Tier 1 and Tier 2. Use the Formulary Advisor. Or call the VA Pharmacy Benefits line at 1-800-877-8339. They handle 18,000 calls a day.
- “My new drug was denied.” Check the monthly decision newsletter. The VA publishes changes every month. If your drug was removed, there’s usually a clinical or cost reason-and an alternative listed.
What’s Changing in 2026?
The VA isn’t standing still. By Q3 2026, the system will start using AI to suggest generic alternatives directly in your provider’s electronic record. If your doctor tries to prescribe a brand-name drug when a generic exists, the system will pop up a prompt: “Consider generic equivalent.” The VA is also expanding access to specialty drugs for rare diseases and cancer. But it’s doing so carefully-balancing cost and need. Expect more transparency: real-time formulary status updates in e-prescribing systems will show you and your provider exactly what’s covered before the prescription is sent.Final Takeaway: Know Your Formulary, Save Money
The VA formulary isn’t perfect. Some newer drugs take longer to get approved. Some veterans still struggle with access to weight-loss or mental health medications outside narrow criteria. But here’s the truth: if you’re using the VA, you’re getting one of the most affordable, well-managed prescription systems in the country. You pay less than 60% of what commercially insured patients pay for the same drugs. You get free delivery. You get expert pharmacists on standby. Your job? Know your meds. Check the formulary. Ask questions. Use Meds by Mail. And don’t assume a brand name is better-because in the VA system, it almost never is.Are all generic medications covered by the VA?
Not every generic is automatically covered. The VA only includes generics that have been reviewed for safety, effectiveness, and cost. If a generic exists but isn’t on the formulary, it’s usually because the VA hasn’t yet evaluated it-or it’s being held for clinical review. Always check the VA Formulary Advisor before assuming coverage.
Can I get brand-name drugs through the VA?
Yes, but only if there’s a documented medical reason. Examples include severe allergies to inactive ingredients in the generic, absorption issues, or a proven lack of effectiveness with the generic version. You’ll need prior authorization from your provider, and the VA will review the request based on clinical guidelines.
How often does the VA update its formulary?
The VA updates its formulary monthly. New drugs are added, restrictions are changed, and tier placements may shift. These updates are published in the VA National Formulary Monthly Decision Newsletter. You can sign up for email alerts on VA.gov or check the Formulary Advisor for real-time changes.
Is Wegovy covered by the VA for weight loss?
Wegovy is covered only for specific FDA-approved uses: type 2 diabetes, cardiovascular disease prevention, or metabolic-associated steatohepatitis (fatty liver disease). It is not covered for general weight loss in veterans without these conditions. This policy changed in January 2025 under updated CHAMPVA guidelines.
What’s the best way to get my VA prescriptions?
For maintenance medications-like those taken daily-Meds by Mail is the easiest and cheapest option. It’s free, no copay, and delivered to your door. For urgent needs or new prescriptions, use your local VA pharmacy. Avoid community pharmacies unless you have prior authorization, as you may pay full price and not be reimbursed.

Kuldipsinh Rathod on 26 December 2025, AT 13:38 PM
Been using VA for 8 years and this formulary saved my ass more than once. Got my blood pressure meds for $3 a month-private insurance wanted $80. No complaints here.