Every year, generic medication errors put patients at risk-not because generics are unsafe, but because the system around them is messy. Around 90% of prescriptions in the U.S. are filled with generic drugs. They save billions and work just as well as brand names. But here’s the problem: when a pharmacist grabs the wrong generic version, or the label doesn’t match what the patient expects, things go wrong fast.
Why Generics Are More Error-Prone
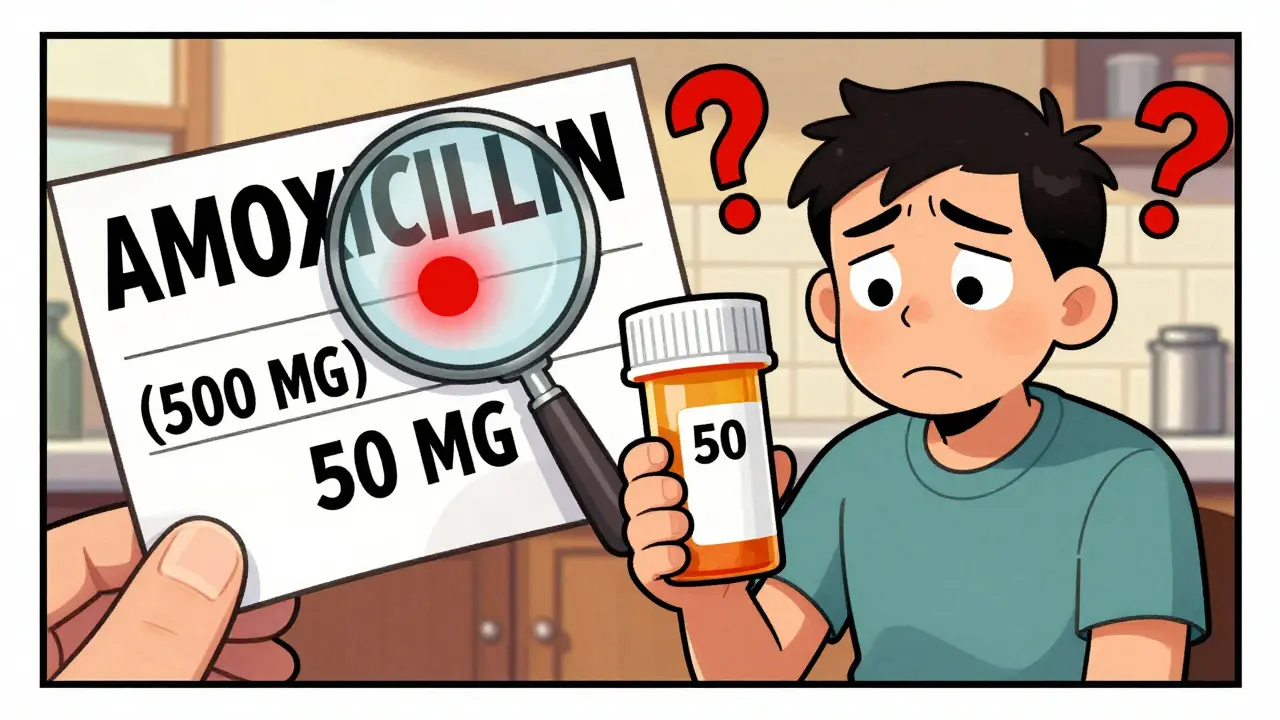
Generics aren’t just cheaper copies-they’re made by dozens of different manufacturers. One pill might be a small white oval from Company A, another a large blue capsule from Company B. Both contain the same active ingredient, but they look completely different. Patients notice. And when they do, they get confused. They think the medicine changed. They stop taking it. Or worse-they double up because they think the new pill is weaker. Then there’s the naming. Look-alike, sound-alike names like Hydralazine and Hydroxyzine are easy to mix up. Add in multiple generic brands with similar packaging, and even experienced pharmacists can slip. A 2007 study found that 14.4% of all prescription corrections were due to dispensing form issues-meaning the pill’s shape, color, or size didn’t match what the patient was used to. And it’s not just the pills. Dosing instructions can be wrong. One generic version might say "take twice daily," another says "take twice weekly." A patient on the wrong one could overdose. That exact mistake happened in a documented case where a patient was given a twice-weekly dose labeled as twice-daily. They ended up in the hospital.Where Errors Happen: The Most Common Mistakes
Pharmacy errors with generics fall into clear patterns:- Dosage errors (37.4% of clinical errors): Wrong strength, wrong frequency. Often from misreading handwritten scripts or outdated digital references.
- Strength discrepancies (19.2%): Prescribing 10mg but dispensing 20mg because the generic bottle was mislabeled.
- Dispensing form issues (14.4%): Giving a different manufacturer’s version without warning. Patient panics. Refuses to take it.
- Quantity mistakes (11.3%): Dispensing 30 pills instead of 90. Or vice versa.
How Technology Helps (and Hurts)
Computerized systems can cut medication errors by up to 55%. That’s huge. But not all systems are built the same.- CPOE (Computerized Physician Order Entry): Reduces errors when doctors type orders instead of scribbling them. But if the system doesn’t flag generic substitutions correctly, it’s useless.
- BCMA (Bar Code Medication Administration): Scanning pills and patient wristbands cuts adverse events by 50%. Still, only 35-40% of community pharmacies use it. Most hospitals do.
- Clinical Decision Support (CDSS): Alerts for drug interactions, duplicates, or wrong doses. Great-until you get 50 alerts a shift. Pharmacists start ignoring them. That’s alert fatigue. And when it happens, the system fails.

What Pharmacists Can Do Right Now
You don’t need fancy tech to prevent errors. You need habits.- Use the 8 R’s every time: Right patient, right drug, right dose, right time, right route, right reason, right documentation, right response. Skip one, and you’re gambling.
- Always check the manufacturer and appearance. If the pill looks different from last time, verify. Don’t assume it’s the same.
- Counsel on first fills. Mandatory counseling for new prescriptions-especially generics-catches 12-15% of errors. That’s one in eight mistakes prevented just by talking to the patient.
- Update your references. Use tools like Drug Facts and Comparisons or Epocrates. Update them yearly. Outdated info is a silent killer.
What Patients Need to Know
Patients aren’t the enemy. They’re the last line of defense.- They should always ask: "Is this the same medicine I took before?"
- If the pill looks different, they should ask why.
- If they feel different after switching, they should tell their pharmacist-immediately.
Fixing Errors When They Happen
Mistakes happen. The goal isn’t perfection-it’s quick correction.- Report every error. Only 28% of community pharmacies track errors formally. That’s dangerous. You can’t fix what you don’t measure.
- Reconcile medications at discharge. When patients leave the hospital, their meds change. Pharmacists who review all their prescriptions-brand and generic-catch an average of 2.3 errors per patient.
- Call the prescriber. If a generic substitution could cause harm-like a patient with a known allergy to a filler in one brand-call the doctor. Don’t wait.

What’s Next: AI and the Future
Pilot programs are testing AI that predicts which patients might react poorly to a specific generic based on their genetics, past reactions, or even their diet. Early results show 22% fewer errors than standard systems. But the real solution isn’t tech. It’s culture. Pharmacies need to stop treating generics as interchangeable commodities. They’re not. They’re different products with different fillers, different shapes, different risks. Treating them like they’re all the same is how mistakes happen. The WHO predicts that if we use existing tools properly-CPOE, BCMA, counseling, updated references-we can cut medication errors by 70-75% by 2030. That’s 1.1 million fewer adverse events every year. It’s not magic. It’s discipline.Frequently Asked Questions
Are generic drugs less safe than brand-name drugs?
No. Generic drugs must meet the same FDA standards for safety, strength, quality, and performance as brand-name drugs. The active ingredient is identical. The difference lies in inactive ingredients (like fillers or dyes), which can rarely cause reactions in sensitive patients. Most people experience no difference at all.
Why do generic pills look different each time I refill?
Multiple manufacturers make the same generic drug. Each one uses different colors, shapes, or markings to distinguish their version. This is legal and common. But it confuses patients. Always check the label for the manufacturer name and ask your pharmacist if you’re unsure.
Can switching between generic brands cause side effects?
For most people, no. But some patients with conditions like epilepsy, thyroid disorders, or mental health issues may be sensitive to small differences in absorption or inactive ingredients. If you feel different after a switch-fatigue, dizziness, mood changes-tell your pharmacist. They can help track it and contact your doctor if needed.
How can I prevent errors when picking up my prescriptions?
Always compare the pill to your last refill. Check the name, strength, and manufacturer on the label. Ask: "Is this the same as before?" If it looks different, ask why. Don’t be afraid to speak up. You’re the last person who can catch a mistake before you swallow it.
Do pharmacists get training on generic drug errors?
Basic training is required for licensure, but ongoing education on generics varies by pharmacy. Many pharmacists learn through experience. The best pharmacies provide regular updates on new generic manufacturers, formulation changes, and look-alike/sound-alike risks. Ask your pharmacy if they offer this training-it’s a sign they care about safety.
Next Steps for Pharmacies
If you run a pharmacy:- Start tracking every dispensing error-even near misses. Use a simple log: date, drug, error type, fix.
- Implement mandatory counseling for all first-fill generic prescriptions.
- Update your drug reference tools at least once a year.
- Advocate for better generic tracking in your pharmacy software.
- Ask your suppliers: "Can you tell me which manufacturer this generic comes from?" If they don’t know, find one who does.
- Keep a list of your meds-including manufacturer names if you know them.
- Ask your pharmacist: "Is this the same as last time?"
- Report any changes in how you feel after switching generics.




Cassie Widders on 12 January 2026, AT 11:22 AM
I’ve had this happen twice-got a blue pill instead of white, panicked, thought my anxiety med was changed. Turned out it was just a different maker. I wish pharmacists would just write a sticky note like the article says. Ten seconds saves so much stress.
Also, why do they never tell you the manufacturer? It’s right there on the bottle, but no one points it out.