Every year, over a million people in the U.S. end up in the emergency room because of medication mistakes. Not because they were careless, but because the system made it easy to get it wrong. You might think, medication safety is just about following the label. But it’s deeper than that. It’s about knowing when to double-check, who to ask, and what to watch for-even when you’re alone in your kitchen at 7 a.m. with a cup of coffee and a handful of pills.
Right Patient: Don’t Assume It’s Yours
The first rule sounds obvious: make sure the medicine is meant for you. But in hospitals, even with barcode scanners, nurses still mix up patients with similar names. At home, it’s worse. Kids grab their parent’s blood pressure pills. Grandparents take a pill that looks like theirs but isn’t. The fix isn’t complicated: always check two things before you swallow anything-your full name and your date of birth. If you’re taking meds at home, keep them in their original bottles. Don’t dump them into pill organizers unless you’ve double-checked each one against the prescription label. And if someone else gives you a pill-your partner, your caregiver, even your adult child-ask them to read the label out loud. Don’t just trust their word.Right Drug: Look Beyond the Brand Name
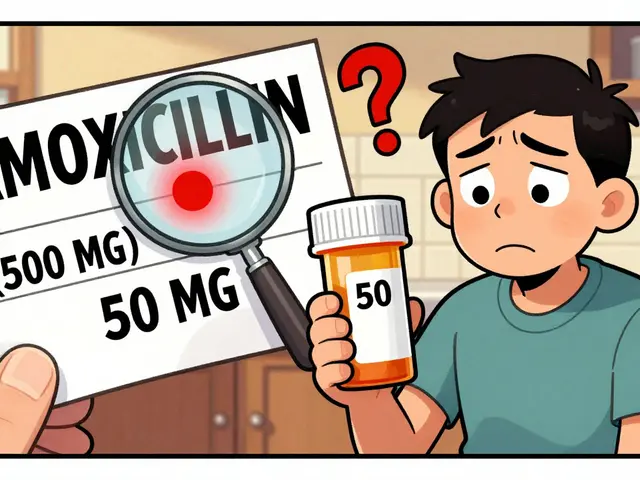
You know your blood pressure pill as “Lipitor.” But the bottle might say “atorvastatin.” That’s the same thing. But what if you’re handed “Lanoxin” instead of “Lisinopril”? They sound alike. They look alike. And mixing them up can send you to the hospital. This happens more than you think. The Institute for Safe Medication Practices says about 25% of medication errors involve look-alike or sound-alike drugs. Always check the generic name on the label. If you’re unsure, ask your pharmacist: “Is this the same as the one I took last month?” Keep a list of your meds-not just names, but why you take them. That way, if you’re rushed or confused, you’ve got a reference. And if you get a refill that looks different, don’t assume it’s just a new batch. Call your pharmacy. It’s not a bother. It’s your life.Right Dose: It’s Not One-Size-Fits-All
A pill that’s perfect for your neighbor might be dangerous for you. Dose depends on your weight, your kidney function, your age, even what else you’re taking. Insulin, blood thinners, and opioids are especially risky. One wrong milligram can cause a bleed, a fall, or worse. If you’re on any of these, always have someone else verify the dose-your pharmacist, a nurse, even a trusted friend. For older adults, a common mistake is cutting pills without knowing if they’re safe to split. Some pills are time-release. Splitting them can release the whole dose at once. And don’t guess. If your doctor says “take half,” they should give you a half-dose tablet. If they don’t, ask. Also, watch for units. “mg” and “mcg” look similar. One is a thousand times stronger than the other. A single typo in a prescription can be deadly. Always read the dose out loud before you take it.
Right Route: Swallowing vs. Injecting
This is where people get hurt without realizing it. A cream meant for your skin shouldn’t go in your mouth. An injection meant for your vein shouldn’t go under your skin. And a suppository isn’t a pill. The Agency for Healthcare Research and Quality found that 16% of medication errors involve the wrong route. At home, this often happens with insulin pens, patches, or eye drops. You’ve got a bottle that says “for external use.” But you’re tired. You’re in pain. You think, “This feels like it should go inside.” Don’t. Always read the instructions. If you’re not sure how to use it-patch, spray, inhaler, eye drop-ask your pharmacist to show you. Do it in front of you. Then do it yourself. Repeat it back. If you’re using an inhaler and it doesn’t feel right, stop. Ask. It’s not embarrassing. It’s smarter than risking lung damage or an overdose.Right Time: Timing Matters More Than You Think
Some meds work best on an empty stomach. Others need food. Some have to be taken every 8 hours. Others, every 12. Missing a dose by an hour might not matter. Missing it by 4 hours might make your blood pressure spike or your seizure return. For time-critical drugs like antibiotics or heart meds, being off by more than 30 minutes can reduce effectiveness. And if you’re on multiple meds, the timing gets messy. A 2022 Kaiser Family Foundation survey found that 61% of seniors over 65 had at least one confusion incident with their meds in the past year. Use a pill organizer with alarms. Use your phone. Set two alarms-one for when to take it, one as a backup. And if you forget? Don’t double up unless your doctor says so. If you’re unsure, call your pharmacist. They’re trained to handle this. They’ve seen it before. Don’t guess. Don’t panic. Just ask.What They Don’t Tell You: The Hidden Rules
The Five Rights are the foundation, but safety doesn’t stop there. There are three more you should know:- Right reason: Why are you taking this? If your doctor prescribed it for anxiety, but you’re now using it to sleep, that’s a problem. Always know the purpose.
- Right response: Are you feeling better? Worse? Any new rashes, dizziness, or nausea? These aren’t side effects to ignore-they’re signals. Report them.
- Right documentation: Keep a written list of every pill, patch, and injection you take. Include the dose and why. Update it every time something changes. Bring it to every appointment-even if you think you remember.
Also, check expiration dates. A 2023 study found that 1 in 5 seniors kept expired meds in their drawers. Some still work. Others break down into harmful chemicals. And never take someone else’s pills-even if they have the same condition. Their dose, their body, their history-it’s all different.
What Works at Home
You don’t need a hospital to stay safe. Simple habits make a huge difference:- Use a pill organizer with compartments for morning, afternoon, evening, and night.
- Download a free app like Medisafe or MyTherapy. They send reminders and let you track side effects.
- Do a “brown bag check” once a month: Dump all your meds into a bag and take them to your pharmacist. They’ll spot duplicates, interactions, and expired pills.
- Ask your doctor to review your meds every six months. If you’re on five or more, this isn’t optional-it’s essential.
- Make sure your home is well-lit when you take meds. Poor lighting causes 37% of seniors to grab the wrong bottle.
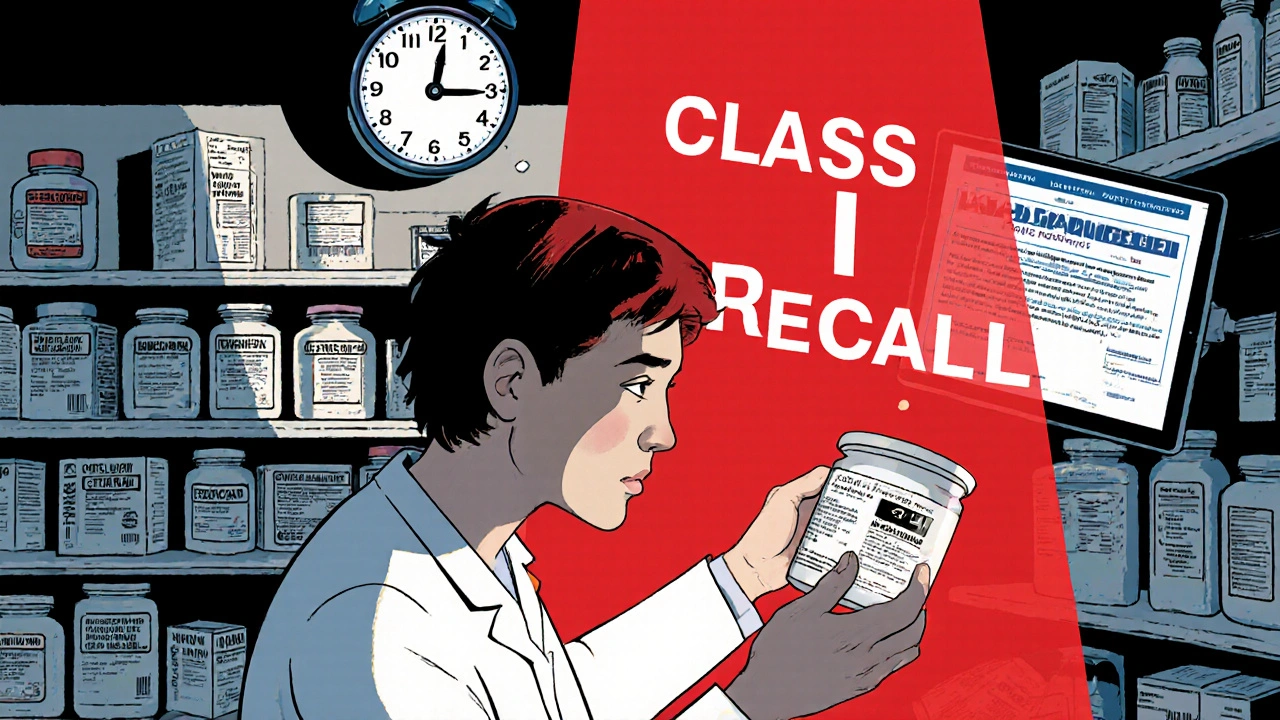
When to Speak Up
You’re the last line of defense. No nurse, no pharmacist, no AI system can replace your eyes and your voice. If something feels off-- The pill looks different
- The label doesn’t match what you remember
- You’re told to take it differently than before
- You’re given a new med without explanation
-stop. Ask. Say: “Can you explain why I’m taking this? What’s it for? What side effects should I watch for?” If you don’t get a clear answer, ask again. Or go to another pharmacist. You have the right to understand your own care. No one should make you feel silly for asking.
What should I do if I accidentally take the wrong medication?
Don’t panic. Don’t induce vomiting unless instructed. Call your pharmacist or poison control immediately (1-800-222-1222 in the U.S.). Have the pill bottle ready-note the name, dose, and how much you took. If you feel dizzy, nauseous, or have chest pain, call 911. Most errors are caught before they cause harm if you act fast.
Can I crush my pills if I have trouble swallowing them?
Only if the label or your pharmacist says it’s okay. Many pills-especially extended-release ones-are designed to release slowly. Crushing them can release the full dose at once, which can be dangerous. If swallowing is hard, ask your doctor for a liquid form, a patch, or a different pill. Never assume it’s safe to crush.
Why do I need to know the generic name of my medicine?
Brand names change depending on who makes the pill. Generic names stay the same. If you know your blood pressure pill is “amlodipine,” you’ll recognize it no matter the brand. This helps avoid duplicates and ensures you’re getting the right drug when switching pharmacies or getting refills.
Is it safe to take medicine past its expiration date?
Most expired meds lose potency but aren’t toxic. However, antibiotics, insulin, nitroglycerin, and liquid suspensions can become unsafe or ineffective. If it’s been more than a year past the date, or if it looks discolored, smells odd, or has changed texture-throw it out. Don’t risk it.
How do I know if my meds are interacting with each other?
Ask your pharmacist to run a drug interaction check every time you get a new prescription. Many interactions don’t show symptoms until they’re serious. Common ones include blood thinners with NSAIDs (like ibuprofen), or statins with grapefruit juice. Keep a full list of everything you take-including vitamins, supplements, and herbal teas-and review it every six months.




Jay Tejada on 5 January 2026, AT 11:58 AM
This post hit me right in the feels. I’ve been giving my mom her meds for two years now, and I still double-check every bottle like it’s a bomb defusal. Turns out, I’m not crazy-just smart.
One time she tried to take her blood thinner like it was a gummy vitamin. I nearly had a heart attack.
Don’t let anyone tell you it’s overkill. It’s survival.