Have you ever taken a pill with your breakfast and wondered if it was working? Or skipped your morning dose because you didn’t want to wait an hour before eating? You’re not alone. For many people, figuring out when to take medication - with food, before food, or on an empty stomach - feels confusing, even overwhelming. But this isn’t just about convenience. Getting the timing wrong can mean your medicine doesn’t work at all… or worse, causes harm.
Why Food Changes How Medicines Work
Food isn’t just fuel. It’s a chemical event in your body. When you eat, your stomach starts churning, your intestines prepare to absorb nutrients, and your bile flows to break down fats. All of this changes how drugs move through your system.Take a simple example: Levothyroxine is a synthetic thyroid hormone used to treat hypothyroidism. It’s designed to be absorbed in the upper small intestine. But if you take it with coffee, milk, or even a bowl of oatmeal, calcium and fiber can bind to it like glue - blocking up to 55% of the dose from entering your bloodstream. That’s why doctors insist on taking it first thing in the morning, with water, at least 30 minutes before eating.
On the flip side, some drugs need food to work. Griseofulvin is an antifungal used for nail infections. Without fat, it barely gets absorbed. But take it with a peanut butter sandwich or a spoonful of olive oil, and absorption jumps by 200-300%. The fat triggers bile release, which dissolves the drug so your body can use it.
Food affects two main things: how fast the drug gets into your blood (rate), and how much gets in (extent). For some drugs, a delay doesn’t matter. For others, it’s the difference between healing and hospitalization.
When Food Slows Down Absorption
Most meals slow down how quickly your stomach empties. A high-fat meal - think bacon, cheese, fried food - can delay gastric emptying by 1.5 to 2 hours. That’s a long time when you’re waiting for a painkiller to kick in.
Acetaminophen is a common pain reliever and fever reducer. On an empty stomach, peak levels hit in about 45 minutes. With a heavy meal? It takes 90 to 120 minutes. For occasional headaches, that delay might not matter. But if you’re in severe pain after surgery, waiting two hours isn’t acceptable.
This delay also affects antibiotics. Tetracycline and Doxycycline are broad-spectrum antibiotics used for acne, urinary infections, and Lyme disease. They bind tightly to calcium, magnesium, and iron - minerals found in dairy, antacids, and even fortified cereals. A glass of milk can slash absorption by 50-75%. That’s why you’re told to avoid dairy for two hours before and after taking these pills. One Reddit user, u/ThyroidWarrior, shared how their recurring UTI only cleared up after they stopped taking doxycycline with their morning yogurt.
When Food Helps Absorption
Not all food is the enemy. Some drugs literally can’t do their job without it.
Nitrofurantoin is an antibiotic for urinary tract infections. Food boosts its absorption by 40%. The same goes for Cefpodoxime, a cephalosporin antibiotic - absorption jumps 50-60% with food. Taking these on an empty stomach doesn’t just make them less effective; it increases the chance of treatment failure and antibiotic resistance.
Sulfonylureas like Glipizide are oral diabetes medications. They trigger insulin release. If you take them without eating, your blood sugar can crash below 70 mg/dL - leading to shaking, sweating, confusion, or even loss of consciousness. The American Diabetes Association found that 23% of patients on these drugs who took them on an empty stomach had to seek emergency care for hypoglycemia. The fix? Take them 30 minutes before your meal. That way, insulin rises just as glucose from food enters your bloodstream.
Even newer drugs like Semaglutide (Ozempic, Wegovy) need careful timing. Novo Nordisk’s 2022 trial showed that taking it within 30 minutes of eating cuts absorption by 44%. That’s why the label says: take it at least 30 minutes before your first bite.

What "With Food" Really Means
"Take with food" sounds simple. But it’s not always about a full meal.
A 2023 Express Scripts report found that 45% of patients misunderstand this instruction. Many think they need a big breakfast. But for some drugs - like certain HIV medications or cholesterol pills - a small snack of 200-300 calories is enough. A banana, a handful of nuts, or a slice of toast can do the trick. Too much food, especially high-fat, can actually delay absorption for some drugs.
Here’s what the experts say:
- Take with food: Within 30 minutes of starting your meal. This applies to drugs like Atorvastatin (Lipitor), Ritonavir, and Itaconazole (when taken with a light meal).
- Take on empty stomach: At least one hour before, or two hours after, eating. This is critical for Levothyroxine, Alendronate (Fosamax), and Levothyroxine.
- Take immediately after food: For drugs like Metformin (Glucophage) - to reduce stomach upset. You don’t need a big meal; just something in your stomach.
Why Timing Matters More Than You Think
It’s not just about effectiveness. Poor timing leads to real-world consequences.
A 2022 meta-analysis in the Journal of Clinical Pharmacy and Therapeutics found that 30% of treatment failures for certain drugs were linked to incorrect food timing. For chronic conditions like thyroid disease or diabetes, that means ongoing symptoms, unnecessary tests, and extra doctor visits.
And the costs add up. Medication-related problems cost the U.S. healthcare system over $500 billion a year. Food-drug interactions contribute an estimated 8% of that - roughly $40 billion. Most of it is preventable.
Older adults are especially at risk. People on five or more medications have a 65% higher chance of having a food-drug interaction. A 72-year-old taking levothyroxine, a blood thinner, a statin, and a calcium supplement might unknowingly be canceling out half their thyroid dose every morning.
How to Get It Right - Practical Tips
Here’s what works in real life:
- Read the label. Don’t assume. Look for phrases like "take on empty stomach," "take with food," or "avoid dairy."
- Use phone alarms. Set one for 60 minutes before breakfast if you take levothyroxine. Set another for 30 minutes before lunch if you take glipizide.
- Keep a food-medication log. Write down what you ate and when you took your pill. After a week, you’ll spot patterns. Did your blood pressure spike after taking lisinopril with a salty sandwich? Did your stomach feel better when you took ibuprofen with toast?
- Ask your pharmacist. They’re trained for this. A 2022 study showed patients who got food-timing advice from their pharmacist had 35% better adherence after 90 days.
- Use apps. Apps like Medisafe and MyTherapy now include food-timing reminders. Users who turned them on saw 27% fewer timing errors.
- Be consistent. If you take your pill with breakfast one day and on an empty stomach the next, your body doesn’t know what to expect. Consistency beats perfection.
For NSAIDs like ibuprofen or naproxen, taking them with food reduces stomach irritation by up to 70%. One GoodRx survey found that stomach pain dropped from 42% to 12% when people followed this advice.
The Future: Personalized Timing
Science is moving beyond one-size-fits-all. In 2023, a Lancet Digital Health study tested levothyroxine timing based on individual gastric emptying rates - measured with a simple breath test. Patients who timed their dose to their unique digestion pattern saw 22% better thyroid hormone levels.
Companies like Medtronic are testing ingestible sensors that track stomach pH and emptying in real time. Imagine a pill that sends a signal to your phone: "Your stomach is ready. Take your pill now."
And it’s not just food. New research in Nature Medicine (March 2024) shows that timing meds to your body’s natural rhythms - like taking blood pressure pills at bedtime - can boost effectiveness by up to 30%. The future is personal.
Can I take my medication with coffee or tea?
It depends. Coffee can interfere with some drugs. For example, it reduces absorption of levothyroxine and some antibiotics. Tea, especially black or green tea, contains tannins that can bind to iron and some antibiotics. The safest rule: take medications with plain water. Wait at least 30 minutes before drinking coffee or tea.
What if I forget and take my pill with food?
Don’t panic. If you took a pill that should’ve been on an empty stomach (like levothyroxine) with food, don’t take another dose. Wait until tomorrow and follow the correct timing. For drugs that need food (like sulfonylureas), taking them without food might cause low blood sugar - so monitor symptoms. If you’re unsure, call your pharmacist. They can tell you if a one-time mistake is risky.
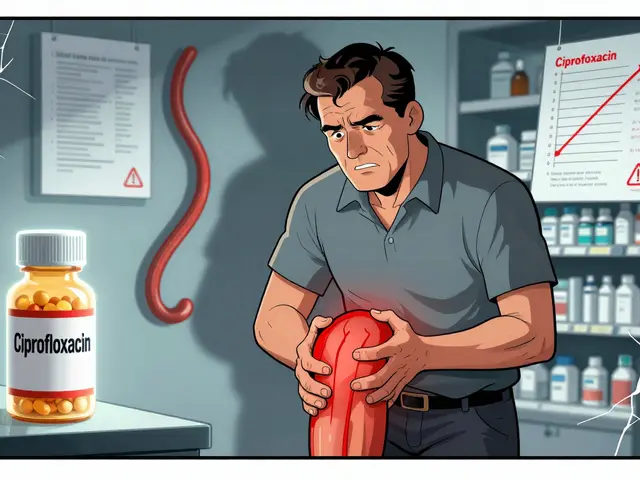
Do I need to avoid all dairy if I’m on antibiotics?
Only for certain antibiotics - mainly tetracycline, doxycycline, and ciprofloxacin. These bind to calcium. Avoid milk, yogurt, cheese, and calcium-fortified juices for at least two hours before and after taking them. Other antibiotics like amoxicillin or azithromycin aren’t affected by dairy.
Why do some pills say "take with a full meal" and others say "take with a light snack"?
It’s about the drug’s chemistry. Some drugs, like itraconazole, need acid in the stomach to dissolve - and high-fat meals raise stomach pH, making them less effective. Others, like certain antivirals, need fat to dissolve properly. A light snack (200-300 calories) is enough to trigger bile flow without slowing digestion too much. Always follow the label - it’s based on clinical trials.
Are there apps that remind me when to take my pills with food?
Yes. Apps like Medisafe, MyTherapy, and Medisafe have built-in food-timing reminders. You can set them to alert you 30 minutes before meals, or 60 minutes before taking a pill on an empty stomach. Users who activated these features saw 27% fewer timing errors in 2023. These tools are especially helpful for people on multiple medications.
Final Thought: Your Body Knows the Rhythm
Medications aren’t magic bullets. They’re chemicals that interact with your body’s natural processes - digestion, hormones, circadian rhythms. Food isn’t the enemy. It’s a partner. The goal isn’t to avoid meals. It’s to align your medicine with your life.
Take your pill at the same time every day. Know whether it needs food or not. Use alarms. Ask your pharmacist. And remember: a small change in timing can mean a big difference in how you feel.