Getting the right medicine is only half the battle. The other half? Making sure you understand exactly what you’re taking. Every year, thousands of people in the U.S. end up in the hospital because they took the wrong dose of a medication - not because the pharmacy made a mistake, but because they didn’t check the label. It sounds simple, but many people miss critical details on their prescription labels, especially when they’re tired, stressed, or dealing with multiple medications. This isn’t about guessing. It’s about knowing exactly what to look for - and how to catch a mistake before it’s too late.
What Does Medication Strength Mean?
When you see 500 mg on your pill bottle, that’s not just a number. It’s the exact amount of active ingredient in each tablet, capsule, or teaspoon of liquid. This is called the strength - and it’s the most important part of your label. A small change here can mean big consequences. For example, 0.5 mg and 5 mg are a tenfold difference. One could be a safe dose for your blood pressure. The other could be dangerous.
Strength is shown differently depending on the form of your medicine:
- Tablets or capsules: "AMOXICILLIN 500 MG" - each pill has 500 milligrams.
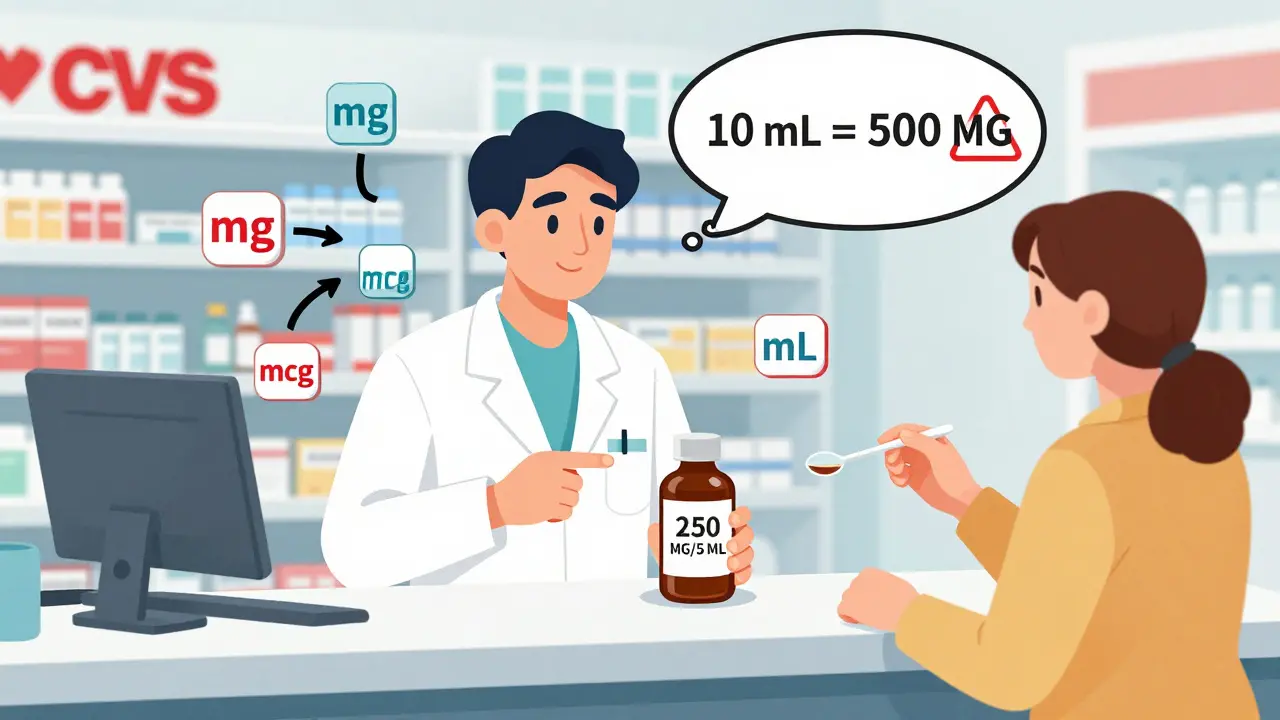
- Liquid medicines: "250 MG/5 ML" - this means 250 milligrams in every 5 milliliters (about a teaspoon). If you give your child 10 mL, you’re giving them 500 mg - double the dose.
- Creams or ointments: "HYDROCORTISONE 1%" - this means 1 gram of medicine in every 100 grams of cream.
Always check the unit. mg (milligrams) is 1,000 times stronger than mcg (micrograms). Mixing them up can be deadly. The FDA banned abbreviations like "U" for units because it looks like "0" - and people have overdosed because of it.
What Does Quantity Mean?
Quantity tells you how much the pharmacy gave you in total. This is not the same as how much you take each day. You might see:
- "30 TABLETS" - that’s the total number of pills you got.
- "120 ML" - the total volume of liquid.
- "30 GRAMS" - the total weight of cream or ointment.
Don’t confuse this with your daily dose. If your doctor says take one pill a day, and you got 30 tablets, that’s a 30-day supply. If you got 90 tablets, that’s a 90-day supply. Always check both the strength and the total amount. If your refill seems way off - too many pills, too little liquid - ask the pharmacist. It’s better to ask than to guess.
Where to Find This Information on the Label
The strength and quantity aren’t hidden. They’re right there - but sometimes hard to read. In the U.S., federal rules require pharmacies to place the strength right next to the drug name. Most chains follow this:
- CVS: Strength appears directly below the drug name.
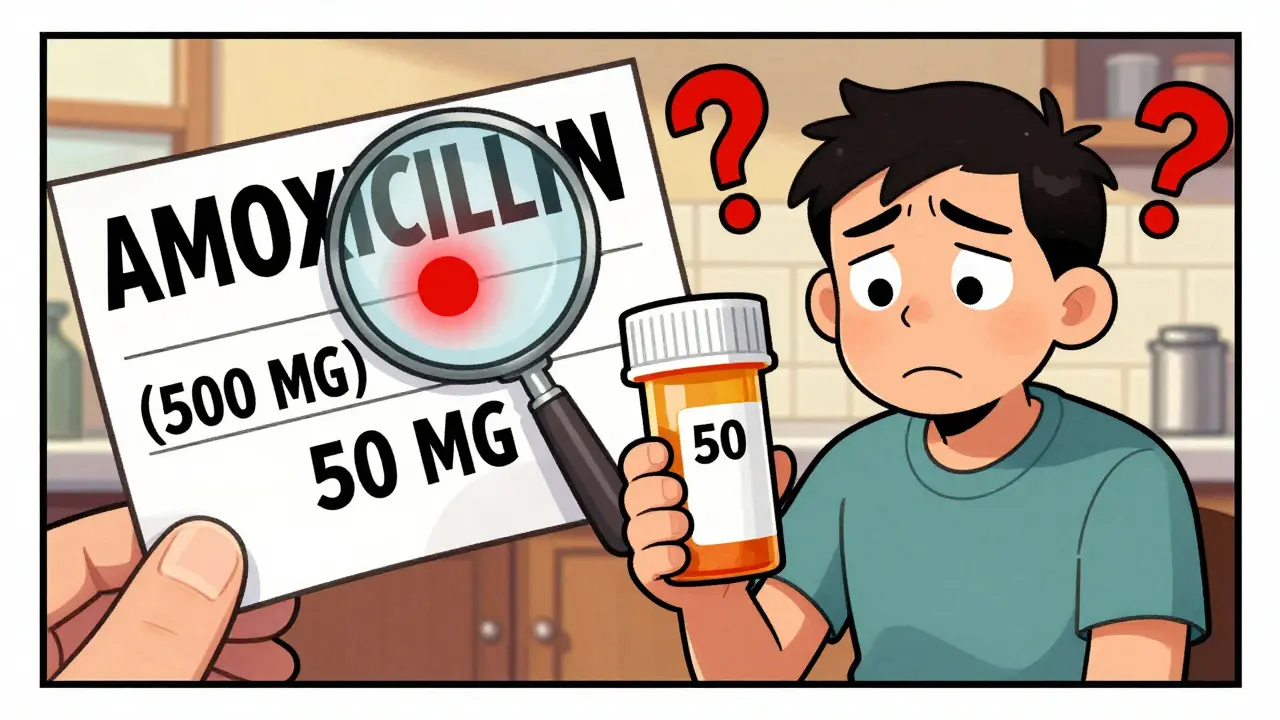
- Walgreens: Strength is in parentheses after the drug name - like "AMOXICILLIN (500 MG)".
- Kaiser Permanente: Some labels include a "Strength Verification" box with a QR code you can scan to see dosage info.
Look for bold text. About 92% of pharmacies use bold to highlight strength. If it’s not bold, that’s a red flag. Also, check the font size. A 2022 survey found 63% of patients said the print was too small. If you can’t read it, ask for a large-print label. Most pharmacies offer it - no extra charge.
How to Verify Your Medication - A 4-Step Check
Don’t just take the label at face value. Use this simple routine every time you pick up a new prescription:
- Find the drug name and strength together. Look for the medication name and the number right beside it. Make sure they’re clearly linked. If the strength is on a separate line or far away, ask if it’s correct.
- Confirm the units. Is it mg? mcg? IU? mL? A single unit mix-up can cause a 100x error. For example, if you’re supposed to take 5 mcg of levothyroxine and get 5 mg, that’s 1,000 times too much.
- For liquids, check the ratio. If it says "5 MG/5 ML", that means 1 mg per mL. If you’re supposed to take 2 mL, you’re getting 2 mg. Write it down: "Total volume = 120 mL. Dose = 5 mL twice a day. That’s 24 doses. Matches the quantity?"
- Match it to your prescription. Did your doctor write "2.5 mg"? Does the label say "10 mg"? That’s a problem. Even if the pill looks different, trust the label - but verify it against what your doctor ordered. If it doesn’t match, go back to the pharmacy.
Pro tip: Keep a small notebook or use your phone to log each prescription - drug name, strength, quantity, and daily dose. You’ll catch mistakes faster.
Common Mistakes and How to Avoid Them
People make the same errors over and over. Here are the top three:
- Misreading decimals: "0.25 mg" looks like "25 mg" if the dot is smudged. Use your phone’s flashlight to zoom in. Or use the magnifier tool on your phone - tap the screen three times and drag the circle over the number.
- Confusing total quantity with daily dose: You got 60 pills. You take 2 per day. That’s 30 days. But if you think "60" means "60 per day," you’re in serious danger. Always ask: "How many should I take each time?"
- Assuming the pill looks right: Pills change color, shape, and size between brands. Just because it looks like last time doesn’t mean it’s the same strength. One man in Arizona took his blood pressure pill for months, thinking it was 2.5 mg - but it was 10 mg. He didn’t know until his heart started racing. The label said "10 MG" - he just didn’t read it.
Experts say patients who check their labels prevent 28% of dosing errors. That’s not luck - it’s a habit.

When Something Doesn’t Add Up
If you spot a mismatch - strength wrong, quantity too high or too low, units unclear - don’t take it home. Go back to the pharmacy. Say: "I’m checking this because I want to make sure it’s right. Can we verify the prescription?"
Pharmacists expect this. In fact, they’re trained to welcome it. A 2023 study found that patients who asked questions were 5 times more likely to catch an error than those who didn’t. And if the pharmacist brushes you off? Ask to speak to the manager. You have a right to know what’s in your medicine.
Some pharmacies now offer free label scanning through their apps. Scan the barcode, and the app will show you the exact strength, dose, and instructions. It’s faster than reading tiny print. CVS, Walgreens, and Rite Aid all have this feature. Turn it on.
What’s Changing in 2025 and Beyond
The FDA is pushing for better labeling. Starting January 1, 2025, all high-risk medications - like insulin, blood thinners, and seizure drugs - must have stronger visual cues. Think red borders around the strength number. Some labels will even use color coding: red for high-alert, yellow for moderate.
Also, NFC chips are being tested. Tap your phone to the label, and it plays a voice recording of your dosage instructions. CVS tried it with 10,000 patients in 2022 - 89% said it helped them feel more confident.
But no technology replaces your eyes and your questions. The most powerful safety tool you have? Your ability to read, understand, and speak up.
Final Reminder
You’re not just a patient. You’re the last line of defense. Pharmacies have systems. Doctors write orders. But if the label says "500 mg" and your doctor meant "50 mg," only you can catch it. Take a second. Look closely. Compare. Ask. It’s not being difficult - it’s being smart.
Medication errors are preventable. But they only stop when you stop accepting things at face value.
What should I do if the strength on my label doesn’t match my doctor’s prescription?
Don’t take the medication. Go back to the pharmacy immediately and ask them to verify the prescription against the original order. Bring your prescription slip or a photo of it if you have one. Most errors happen during transcription - the pharmacy may have misread the doctor’s handwriting or entered the wrong number. Pharmacists are trained to fix this, and they’ll correct it for free.
Can I ask for a larger font on my prescription label?
Yes, absolutely. Under the Americans with Disabilities Act and FDA guidelines, pharmacies are required to provide large-print labels upon request. You don’t need a doctor’s note. Just ask: "Can I get this in large print?" Most chain pharmacies offer this, and it’s free. If they say no, ask for the manager - this is a legal right.
Why does my liquid medicine say "5 mg/5 mL" instead of just "1 mg/mL"?
It’s for safety. Saying "5 mg/5 mL" makes it easier to measure. If you’re told to give 5 mL, you know you’re giving 5 mg. If it just said "1 mg/mL," you’d have to do the math: 5 mL × 1 mg/mL = 5 mg. That’s one more step where mistakes can happen. The FDA recommends keeping the ratio as written on the prescription to reduce confusion.
Is it safe to rely on the pill’s color or shape to know the strength?
No. Pills change shape, color, and size depending on the manufacturer. A blue pill one month might be white the next - but still be the same strength. Or it might be a different drug entirely. Never assume. Always check the label. The only reliable way to know strength is what’s printed on the bottle - not what the pill looks like.
What should I do if I accidentally took the wrong dose?
Call your pharmacist or poison control at 1-800-222-1222 immediately. Don’t wait for symptoms. Even if you feel fine, some overdoses take hours to show up. Have the medication bottle handy - they’ll need the strength, quantity, and your weight. If you’re unsure whether it was an overdose, assume it was. Better safe than sorry.


Gloria Ricky on 9 February 2026, AT 19:55 PM
Just picked up my mom’s new blood pressure med and almost missed the "mcg" vs "mg" thing-thank you for this. I used my phone’s magnifier like you said and caught it before she took it. She’s 78 and blind in one eye, so I’m glad I checked. Small things save lives.