Every time you pick up a bottle of medicine-whether it’s from the pharmacy counter or the shelf at the grocery store-you’re holding a safety manual. But most people skim it like a receipt. That’s dangerous. Medication labels aren’t just paperwork. They’re your lifeline to taking the right dose, at the right time, without risking harm.
What’s Actually on the Label?
Prescription and over-the-counter (OTC) labels look different, but they both give you the same critical info. For prescriptions, the label must include your name, the drug name, the strength, how much to take, how often, and warnings. OTC labels follow the FDA’s Drug Facts format, which is designed to be easy to scan.Here’s what you need to look for, no matter the label:
- Active Ingredient(s): This is the medicine that does the work. It’s listed first, with the amount per dose. For example, “Acetaminophen 500 mg.” If you’re taking more than one medicine, check this section. Many cold and flu pills have acetaminophen too. Taking two could mean you’ve hit a toxic dose.
- Dosage and Directions: This tells you how much to take and how often. “Take one tablet every 6 hours as needed for pain.” It sounds simple, but people mess this up all the time. Don’t assume “every 6 hours” means four times a day-some people take it at 8 a.m., 2 p.m., 8 p.m., and then again at 2 a.m. That’s not safe. Stick to waking hours unless your doctor says otherwise.
- Uses: What the medicine is for. If your symptom isn’t listed, don’t use it. That’s not what it’s designed to treat.
- Warnings: This is the most ignored part. It tells you when NOT to take the drug. Allergies? Liver problems? Pregnancy? Alcohol? If you have any of these, the warning will say so. Skip this, and you could end up in the ER.
- Inactive Ingredients: These don’t treat anything, but they can cause reactions. If you’re allergic to dyes, gluten, or lactose, check here.
- Expiration Date: Medicine doesn’t last forever. Expired pills can lose strength or even break down into harmful chemicals. Don’t use anything past its date.
Why Dosage Is So Tricky
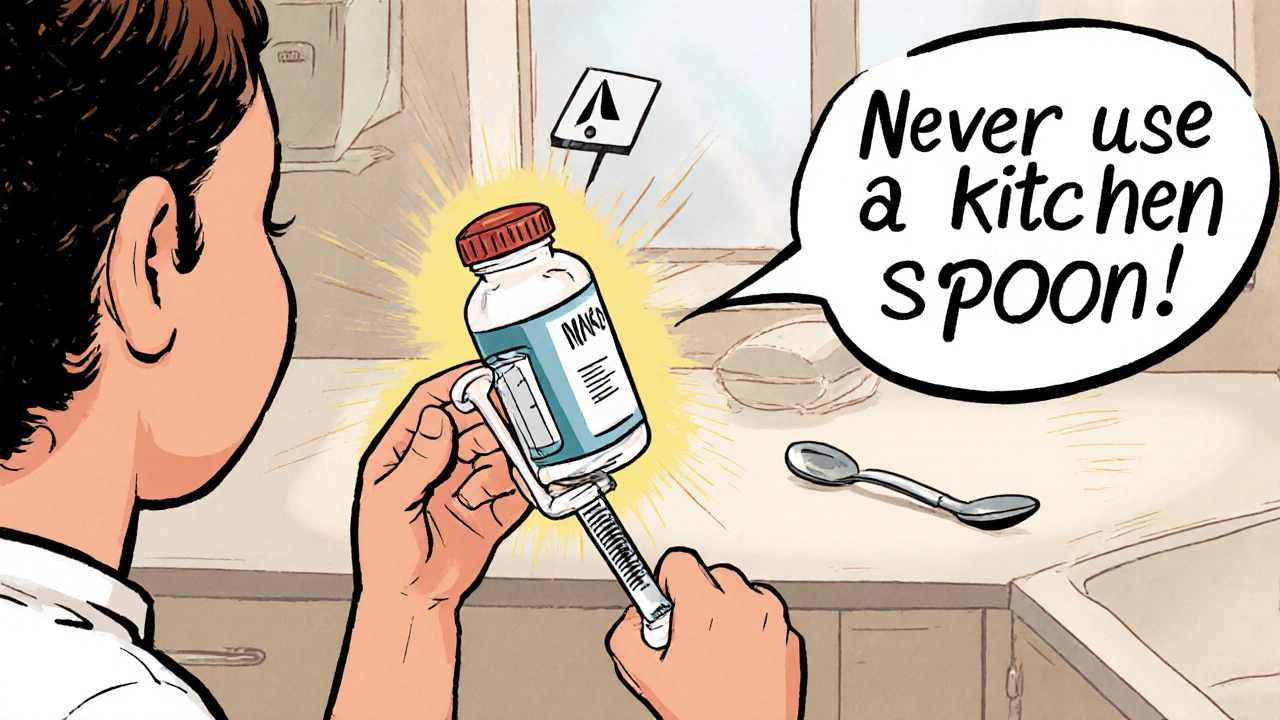
The biggest mistake people make? Misreading how much to take. Liquid medicines are the worst. A label might say: “350 mg per 5 mL.” That means each teaspoon-sized dose (5 mL) has 350 mg. If your doctor says you need 700 mg, you need two doses-not the whole bottle.A 2022 study found that 68% of parents of young children made errors when measuring liquid medicine. Why? They used kitchen spoons. A teaspoon isn’t a teaspoon. One can hold 2.5 mL. Another might hold 7.3 mL. That’s a threefold difference. The American Academy of Pediatrics says: Never use a kitchen spoon. Use the plastic syringe or cup that came with the medicine. If it’s missing, ask the pharmacist for one. They’ll give it to you free.
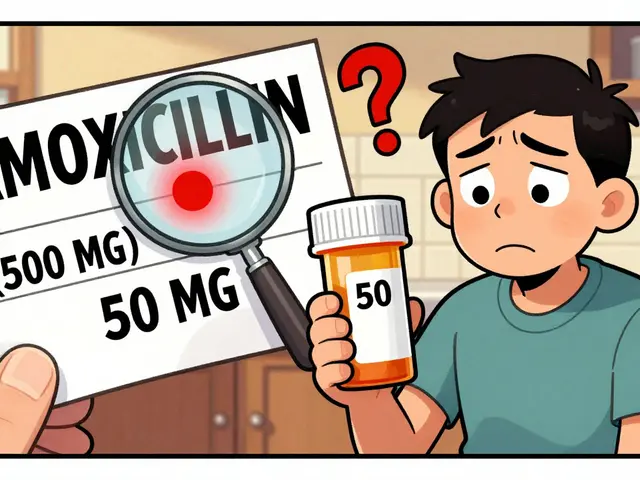
For pills, check the strength. A pill labeled “5 mg” is not the same as “10 mg.” If you’re used to taking one 5 mg pill and your prescription changes to 10 mg, you might think you need two of the old ones. But the new pill is already double the dose. Taking two would be dangerous.
What You’re Probably Missing
Most people look at the dose and move on. But there’s hidden info you need to see.“Take with food” or “Take on an empty stomach”: This matters. Some drugs get absorbed better with food. Others can irritate your stomach if taken without. If it says “take on an empty stomach,” wait two hours after eating. If it says “take with food,” have a snack or meal.
“Do not crush or chew”: Some pills are designed to release slowly. Crushing them can dump the full dose all at once. That’s how people overdose on extended-release opioids or blood pressure meds.
“May cause drowsiness”: If you’re driving, operating machinery, or caring for kids, this warning isn’t optional. Drowsiness can hit even if you’ve taken the medicine before. Your body doesn’t always build tolerance.
“Do not use with alcohol”: Alcohol and painkillers? A deadly mix. Alcohol and antidepressants? Can make you suicidal. Alcohol and antibiotics? Can make you sick. Always check.
Special Cases: Kids, Seniors, and Multiple Medicines
For children, weight matters more than age. A 15-pound baby needs a completely different dose than a 40-pound toddler. Always check the label for weight-based dosing. If it’s not there, ask your pharmacist. Don’t guess.Older adults often take five or more medications. That’s where problems grow. One pill might say “take once daily.” Another says “take twice daily.” You start mixing them up. Use a pill organizer. Write down the schedule. Set phone alarms. If you’re confused, ask your pharmacist to do a “medication review.” They’ll spot duplicates or dangerous interactions.
And here’s the silent killer: duplicate active ingredients. You take Tylenol for your headache. Then you take a cold medicine that also has acetaminophen. You don’t realize it. Now you’ve taken 3,000 mg in one day. The safe limit? 3,000-4,000 mg max. You’re already at the edge. That’s how liver failure starts.
What to Do If You’re Unsure
You don’t have to figure it out alone. Pharmacists are trained to explain labels. They’re not just the people who hand you the bottle. They’re your safety net.If the label doesn’t make sense:
- Call the pharmacy. Ask them to walk you through it.
- Ask for a Medication Guide. For high-risk drugs like blood thinners, opioids, or chemotherapy, the FDA requires a separate printed guide. If you didn’t get one, ask.
- Take the bottle to your doctor or pharmacist and say: “I don’t understand this. Can you show me?”
- Use the FDA’s website or trusted sources like BeMedWise.org to look up the drug name and see the official label.
There’s no shame in asking. In fact, the American Medical Association says that 50% of medication-related hospital visits happen because patients didn’t understand their labels. You’re not the problem. The system is. But you can fix it-for yourself.
What’s Changing Soon
The FDA is working to make labels clearer. By 2024, some prescriptions will start having QR codes. Scan it, and you’ll get a video showing how to take the medicine. Some labels will use icons: a skull for “toxic if misused,” a clock for “take at bedtime.” Color-coding for high-risk drugs is coming too.But you don’t have to wait. Right now, you have everything you need: the label, your eyes, and your voice. Use them.
Final Checklist: Before You Take Any Medicine
Before you swallow anything, run through this:
- Is this medicine for me? (Check your name on the prescription bottle.)
- Is this the right drug? (Does the name match what your doctor told you?)
- Is this the right dose? (Is the number on the label what your doctor prescribed?)
- Is this the right way? (Swallow? Inject? Apply? Use as directed?)
- Is this the right time? (Every 6 hours? After meals? At bedtime?)
- Do I know the warnings? (Any allergies? Alcohol? Other meds?)
- Is it still good? (Check the expiration date.)
If you can answer yes to all seven, you’re safe. If even one is unclear-stop. Call someone.
What if I can’t read the small print on the label?
Ask your pharmacist for a large-print label. Most pharmacies offer this for free. You can also use your phone’s camera to zoom in on the label or take a photo and enlarge it. Some apps, like Medisafe or MyTherapy, let you scan a label and read it aloud. Don’t struggle with blurry text-there are tools to help.
Can I trust the expiration date on my medicine?
Yes, but understand the difference. The manufacturer’s expiration date is the last day the drug is guaranteed to work at full strength. Pharmacies often put their own expiration date on prescription bottles-usually one year from when it was filled. That’s a safety buffer. Even if the bottle says it’s good for two more years, if your pharmacy put a one-year date on it, follow that one. It’s more conservative and safer.
What should I do if I accidentally take too much?
Don’t wait. Call Poison Control at 1-800-222-1222 immediately. Or go to the nearest emergency room. Bring the medicine bottle with you. If it’s an opioid, benzodiazepine, or insulin overdose, time is critical. Don’t try to “wait it out.” Every minute counts.
Why do some labels say “take with water” and others don’t?
It’s not just a suggestion. Some pills can get stuck in your esophagus if you don’t drink enough water. That can cause serious irritation or ulcers. Antibiotics like doxycycline and bisphosphonates for osteoporosis are especially risky. Even if it doesn’t say “take with water,” drink a full glass anyway. It helps the pill go down and reduces side effects.
Is it okay to split pills or open capsules?
Only if the label or your doctor says so. Many pills are coated or designed to release slowly. Splitting them can destroy that design. Capsules with time-release beads shouldn’t be opened-you’ll get the whole dose at once. If you need a lower dose, ask your doctor for a different strength. Don’t guess.
What if I miss a dose?
Check the label. Most will say: “If you miss a dose, take it as soon as you remember. But if it’s almost time for the next dose, skip the missed one.” Never double up unless it says so. For blood thinners, antibiotics, or birth control, missing a dose can be dangerous. If you’re unsure, call your pharmacist.
Next Steps: Make Medication Safety a Habit
Start today. Keep a list of every medicine you take-prescription, OTC, vitamins, supplements. Update it every time you get a new one. Show it to your doctor at every visit. Ask: “Is this still right for me?”Keep your medicines in their original bottles. Never dump pills into a pillbox without knowing what they are. If you’re traveling, bring the original labels with you. If you’re hospitalized, bring your list. You’re your own best advocate.
Medication safety isn’t about being perfect. It’s about being aware. One label, one question, one phone call-could save your life. Don’t skip it.



Joe bailey on 26 November 2025, AT 02:43 AM
Man, I used to just glance at the bottle and go. Until my buddy almost ended up in the ER from mixing Tylenol and cold meds. Now I read every tiny line. Seriously, it’s not that hard. Just take two seconds. Your liver will thank you.
Also, pharmacists? They’re basically superheroes. Never feel dumb asking them to explain it. I’ve had them draw me diagrams. No joke.