Every year, thousands of people accidentally take two doses of the same medication-sometimes within hours of each other. It’s not always a mistake made by someone confused or forgetful. Sometimes it’s a well-meaning parent who gives medicine after a child throws it up. Sometimes it’s an older adult who can’t remember if they took their pill this morning. And sometimes, it’s two different caregivers giving the same dose without knowing the other already did. The result? Nausea, dizziness, liver damage, even death. Double-dosing is one of the most common and dangerous medication errors in homes across the UK and the US-and it’s entirely preventable.
Why Double-Dosing Happens More Than You Think
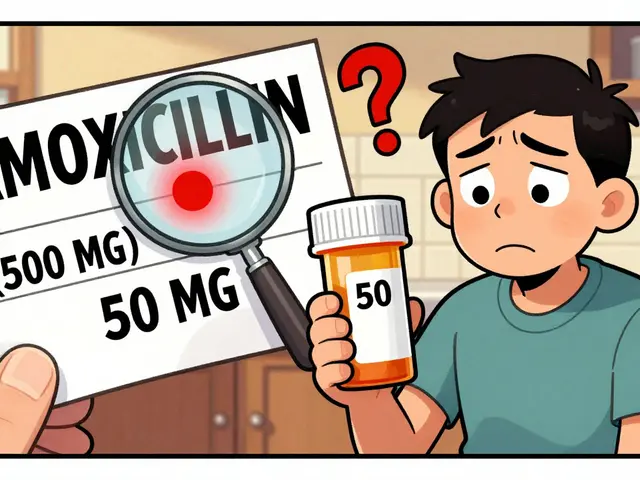
Most people assume they’re careful with their meds. But the data says otherwise. A 2023 survey by WesleyLife found that 28% of seniors admitted to accidentally taking a second dose in the past year. In households with children, 41% of emergency visits for medicine poisoning involved kids taking medication meant for an adult. And in multi-caregiver homes-where a spouse, child, or visiting relative helps with meds-double-dosing incidents jump by nearly 50%. The problem isn’t always forgetfulness. It’s complexity. The average American senior takes 4 to 5 prescription drugs daily. Add in over-the-counter painkillers, vitamins, and supplements, and you’ve got a minefield. Many people don’t realize that Tylenol and cold medicines both contain acetaminophen. Or that ibuprofen shows up in both pain relievers and sleep aids. One dose from each can push you over the safe limit.The Simplest Tool: The Weekly Pill Organizer
If you take more than one pill a day, a pill organizer isn’t optional-it’s essential. Look for one with separate compartments for morning, afternoon, evening, and bedtime. A standard 7-day organizer with four slots per day is the most common and effective type. Sixty-eight percent of seniors use them, and when used correctly, they cut double-dosing by 35%. Here’s how to make it work: Fill it every Sunday. Put each pill in its exact time slot. Don’t skip days. Don’t cram extra pills in because you think you’ll “remember.” Once you’ve taken your dose, look at the compartment. If it’s empty, you’re good. If it’s still full, you haven’t taken it yet. No guessing. No second-guessing. For people who only take one pill a day, flipping the bottle upside down after taking it works too. But for multiple daily doses? A pill box is the only reliable visual cue. It turns memory into sight.Digital Reminders: When Your Phone Becomes Your Medication Buddy
Apps like Medisafe, MyTherapy, and even Apple Health’s medication tracker can be lifesavers. In a 2022 study, users who used these apps saw an 87% improvement in adherence. That means fewer missed doses-and fewer double doses. Set up alerts for each medication at the exact time you need to take it. Some apps let you add notes: “Take with food,” “Don’t lie down after,” or “Only if pain is above 6/10.” You can even add family members as observers. If you miss a dose, the app sends a reminder to someone else. That’s huge in households where more than one person helps with meds. Don’t overcomplicate it. You don’t need a fancy smart dispenser. Just a smartphone, a free app, and 20 minutes to set it up. The key is consistency. Once the alerts become part of your routine-like brushing your teeth-you stop thinking about it. And that’s when safety kicks in.Never Use Kitchen Spoons for Liquid Medications
This one catches people off guard. A teaspoon is not a teaspoon. A kitchen spoon can hold anywhere from 2.5 millilitres to 7.3 millilitres. That’s a 200% variation. If you’re giving a child 5mL of antibiotics and use a random spoon, you could be giving them nearly 8mL. That’s an overdose. Always use the syringe, dropper, or cup that came with the medicine. If you lost it, ask your pharmacy for a replacement-they’ll give you one for free. For adults, use the small plastic measuring cups that come with liquid painkillers. For kids, use the oral syringe with clear markings. No exceptions. And never guess. If the dose says “5mL,” don’t say “that’s about a tablespoon.” It’s not. It’s five millilitres. Precisely.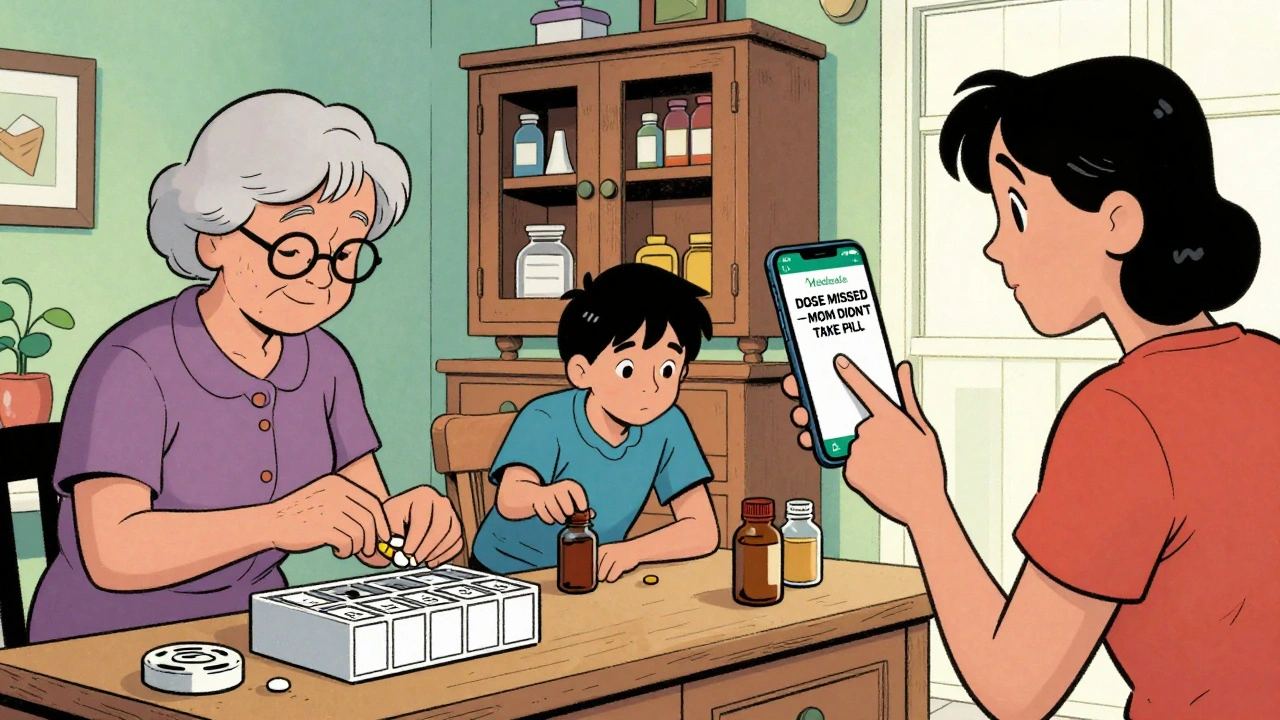
Keep a Master Medication List
Write down every single thing you or your loved one takes. Not just prescriptions. Include:- Over-the-counter pain relievers
- Vitamins and supplements
- Herbal remedies
- Topical creams with active ingredients (like lidocaine or NSAIDs)
Designate One Person to Handle Medications
In homes with multiple caregivers-parents, grandparents, nannies, visiting relatives-confusion is inevitable. One person gives the medicine. Another doesn’t know. So they give it again. That’s how accidents happen. St. Louis Children’s Hospital recommends assigning one person as the official “medication manager.” That person is the only one who gives the medicine. They’re also the only one who updates the list, refills the pill box, and talks to the pharmacist. If someone else wants to help, they ask the manager first. This isn’t about control. It’s about clarity. In households that do this, double-dosing drops by 47%. It’s that simple.Store Medications Out of Reach-and Out of Sight
Children’s Healthcare of Atlanta found that 86% of emergency visits for medicine poisoning involved kids taking medication belonging to a family member. That’s not just accidental ingestion-it’s preventable access. Keep all meds-prescription, OTC, vitamins-in a locked cabinet. Not on the counter. Not in the bathroom. Not in a drawer the child can open. If you have grandchildren visiting, lock it before they come over. Even if you think they’re “too old” to be curious. Kids are curious. Always. Same goes for seniors. If someone has memory issues, don’t leave pills on the nightstand. Put them in the organizer and store it in a safe spot. A locked medicine cabinet is the gold standard.
Use Routines, Not Clocks
Trying to remember “take pill at 8 a.m.” is unreliable. Life doesn’t run on a schedule. What if you’re late? What if you’re away from home? What if your watch dies? Instead, tie your medication to a daily habit you never skip. Brush your teeth? Take your pill right after. Eat breakfast? Take it before. Walk the dog? Take it when you come back. These routines stick better than alarms. In fact, 78% of people who successfully stick to their meds do it by linking them to a routine.What to Do If You Accidentally Double-Dose
If you realize you’ve taken two doses, don’t panic. But don’t wait either. Call 1-800-222-1222 immediately. That’s the National Poison Control Center. They’re free, confidential, and available 24/7. Tell them:- What medication you took
- How much you took
- When you took it
- How old you are
- Any symptoms you’re feeling
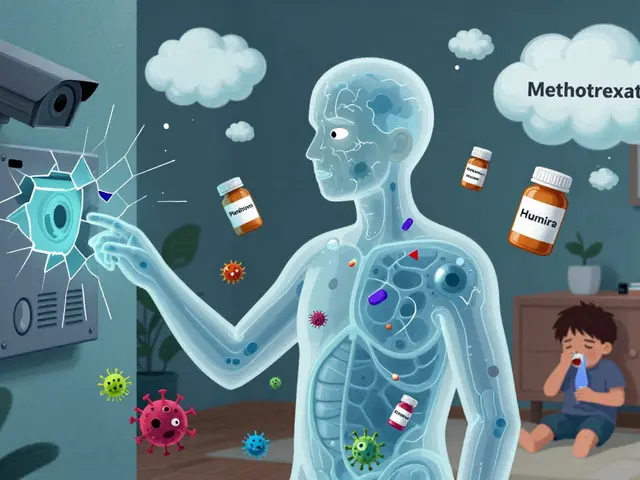
What’s Changing in 2025
New smart pill dispensers are starting to appear in homes. These lock after each dose and send alerts if a dose is missed. One Johns Hopkins study found they cut double-dosing by 76%. They’re still expensive-but some insurance plans now cover them for high-risk patients. AI-powered apps are also coming. By learning your habits, they can warn you if you’re about to take a duplicate dose based on your past patterns. These aren’t science fiction-they’re coming by 2026. But here’s the truth: none of these fancy tools matter if you don’t use the basics. A pill organizer. A medication list. A designated person. A locked cabinet. These are the tools that save lives right now.Final Checklist: Your Daily Safety Routine
- ✅ Use a 7-day pill organizer with AM/PM/PM/Bedtime slots
- ✅ Fill it every Sunday-no exceptions
- ✅ Set a phone reminder for each dose
- ✅ Never use kitchen spoons-only the measuring tool that came with the medicine
- ✅ Keep a written list of every medication, including vitamins and OTCs
- ✅ Assign one person to give all meds in the household
- ✅ Store all meds in a locked cabinet, out of children’s reach
- ✅ Link doses to a daily habit (brushing teeth, eating breakfast, etc.)
- ✅ Save 1-800-222-1222 in your phone as “Poison Control”
Medication safety isn’t about being perfect. It’s about building systems that catch your mistakes before they hurt you. Start with one step. Then another. You don’t need to fix everything today. But if you do one thing this week-like getting a pill organizer-you’ve already made your home safer.
What should I do if I think I took two doses of my blood pressure pill?
Call Poison Control at 1-800-222-1222 right away. Don’t wait for symptoms. Blood pressure medications can cause dangerously low heart rate or dizziness if doubled. They’ll ask you the name of the pill, how much you took, and when. Write that down before you call. Stay calm. Most cases don’t require an ER visit, but you need expert advice.
Can I use a pill organizer for liquid medications?
No. Pill organizers are for solid pills and capsules only. Liquid medications must be measured with the syringe or cup that came with the bottle. Pouring liquids into pill compartments can cause spills, contamination, or inaccurate dosing. Always use the original measuring tool-even if it’s messy. Safety matters more than convenience.
My parent takes 8 different pills a day. Is a weekly organizer enough?
Yes, if it has four compartments per day (morning, noon, evening, bedtime). A 7-day organizer with 4 slots holds up to 28 doses-enough for most regimens. If your parent takes more than four doses a day, ask your pharmacist for a multi-dose dispenser. Some pharmacies offer pre-filled blister packs with dates and times printed on them.
Why do I keep forgetting if I took my pill even with a pill organizer?
You might be filling the organizer incorrectly. Make sure you’re putting the right pill in the right slot. Also, check if you’re moving pills around. Never transfer pills from one compartment to another after taking them. That breaks the visual system. If you’re still unsure, add a digital reminder. Two systems are better than one.
Are there free apps for medication reminders?
Yes. Medisafe, MyTherapy, and Health Reminders (on iOS) are all free and highly rated. They let you add photos of your pills, set multiple alarms, and notify family members if a dose is missed. Download one, spend 20 minutes setting it up, and test it for three days. If it works for you, keep it. If not, try another. There’s no one-size-fits-all app.
What if I’m traveling and can’t use my pill organizer?
Use a small, portable pill case with just the doses you need for the trip. Label it clearly with the day and time. Keep your medication list handy. Set phone reminders for your new time zone. Never rely on memory. If you’re unsure whether you took a dose, wait until the next scheduled time. It’s safer to skip one dose than to risk doubling up.
Can I just use a calendar to track my meds?
A calendar helps, but it’s not enough. You can forget to check it. You can miss a day. You can’t see it at a glance like a pill box. Use a calendar alongside a pill organizer-not instead of it. The visual confirmation of an empty compartment is the most reliable method.
Why do pharmacies give out pill organizers for free?
Because they know it prevents errors-and saves lives. Hospitals and pharmacies lose money when patients end up in the ER due to medication mistakes. Pill organizers reduce those errors, which lowers costs and improves outcomes. Many pharmacies offer them at no cost, especially for seniors or patients on complex regimens. Ask for one next time you pick up a prescription.



Larry Lieberman on 10 December 2025, AT 10:31 AM
Just got my first pill organizer yesterday after reading this. Holy crap, why didn’t I do this sooner? My grandma takes 7 meds and I’ve been winging it with sticky notes. This is a game-changer. 🙌