When your doctor orders a brain MRI, it’s not because they’re being overly cautious-it’s because they need to see what’s happening inside your skull in a way no other test can. Unlike X-rays or CT scans, MRI doesn’t use radiation. Instead, it uses strong magnets and radio waves to create incredibly detailed pictures of your brain’s soft tissues. This makes it the go-to tool for spotting problems like tumors, strokes, multiple sclerosis plaques, and even tiny bleeds that other scans might miss. If you’ve been told you need one, understanding what you’re looking at can take away some of the fear-and help you ask the right questions.
What You’re Actually Seeing on a Brain MRI
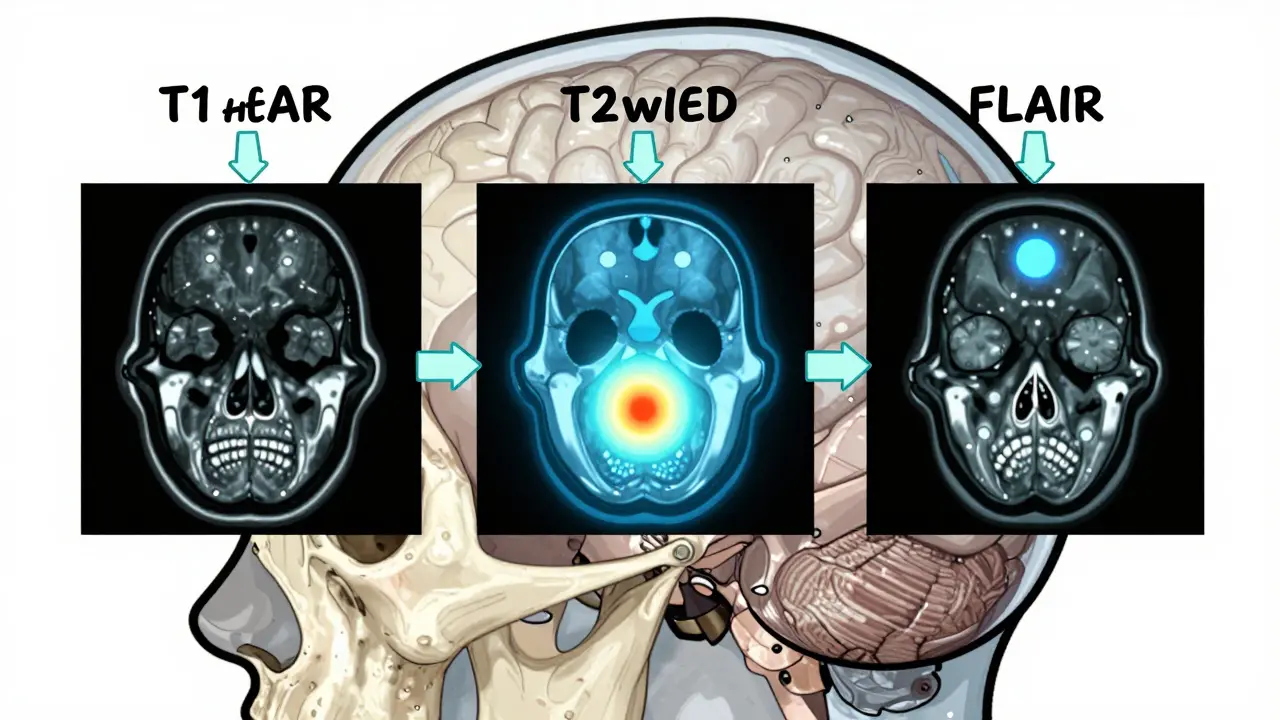
A brain MRI isn’t a single image. It’s a series of pictures, each using a different setting called a pulse sequence. These sequences highlight different things in your brain. Think of them like different camera filters: one shows water, another shows fat, another shows blood. The three most important ones you’ll see are T1-weighted, T2-weighted, and FLAIR.T1-weighted images give you the clearest picture of brain anatomy. On these, fat looks bright white, and fluid like cerebrospinal fluid (CSF) looks dark. This is how radiologists check if your brain’s structure looks normal-like whether your ventricles (the fluid-filled spaces inside your brain) are the right size, or if your gray and white matter are clearly separated. A healthy brain on T1 shows a crisp 30-40% difference in brightness between gray and white matter.
T2-weighted images flip the script. Here, water and anything swollen or inflamed glows bright white. That’s useful because most brain problems-like tumors, infections, or areas damaged by lack of blood flow-contain extra water. But there’s a catch: CSF also glows bright on T2, so it can hide small lesions near the ventricles. That’s why the next sequence is so important.
FLAIR (Fluid-Attenuated Inversion Recovery) is the T2 sequence’s smarter cousin. It turns down the brightness of CSF so that only abnormal tissue stands out. This is the gold standard for spotting multiple sclerosis plaques, which often form near the brain’s ventricles. Without FLAIR, those lesions might disappear into the bright CSF background. Radiologists rely on FLAIR to find even the smallest white matter lesions that could be early signs of neurological disease.
What Common Findings Actually Mean
Not every bright spot on an MRI is a crisis. Many findings are normal for age-or completely harmless. But some need attention.White matter hyperintensities are tiny bright spots, often near the ventricles. They’re common in people over 60. In fact, up to 90% of people over 70 have them. These are usually due to small vessel disease-tiny blood vessels in the brain that have narrowed over time. They’re linked to high blood pressure, diabetes, or aging. While they don’t always cause symptoms, a lot of them can signal increased stroke risk. The key is how many there are and where they’re located.
Lacunar infarcts are tiny strokes, usually less than 5mm wide. They show up as small, round bright spots on T2 and FLAIR, often in the deep parts of the brain like the basal ganglia or thalamus. Many people have them without ever knowing-they’re called “silent strokes.” But if you’ve had a few, your risk of a bigger stroke or dementia goes up. They’re a red flag for uncontrolled hypertension.
Multiple sclerosis plaques are different. They’re usually oval, not round, and often sit perpendicular to the ventricles-a pattern called “Dawson’s fingers.” They’re brighter on FLAIR than T2, and they don’t fade over time like some other lesions. If you’re under 50 and have several of these, especially with neurological symptoms like numbness or vision loss, MS is a real possibility.
Acute stroke shows up fast on a special sequence called diffusion-weighted imaging (DWI). Within minutes of a stroke, water movement in brain cells gets restricted. DWI picks this up immediately. If DWI is bright and the ADC map (a related image) is dark, it’s an acute stroke. This is why MRI is so critical in stroke centers-it can confirm a stroke before CT even shows anything.
Microbleeds are tiny spots of old blood, usually seen on a sequence called SWI or gradient echo. They look like small black dots. They’re common in older adults, especially those with high blood pressure or amyloid angiopathy. Finding more than five microbleeds increases stroke risk. They’re also a warning sign for people considering blood thinners.
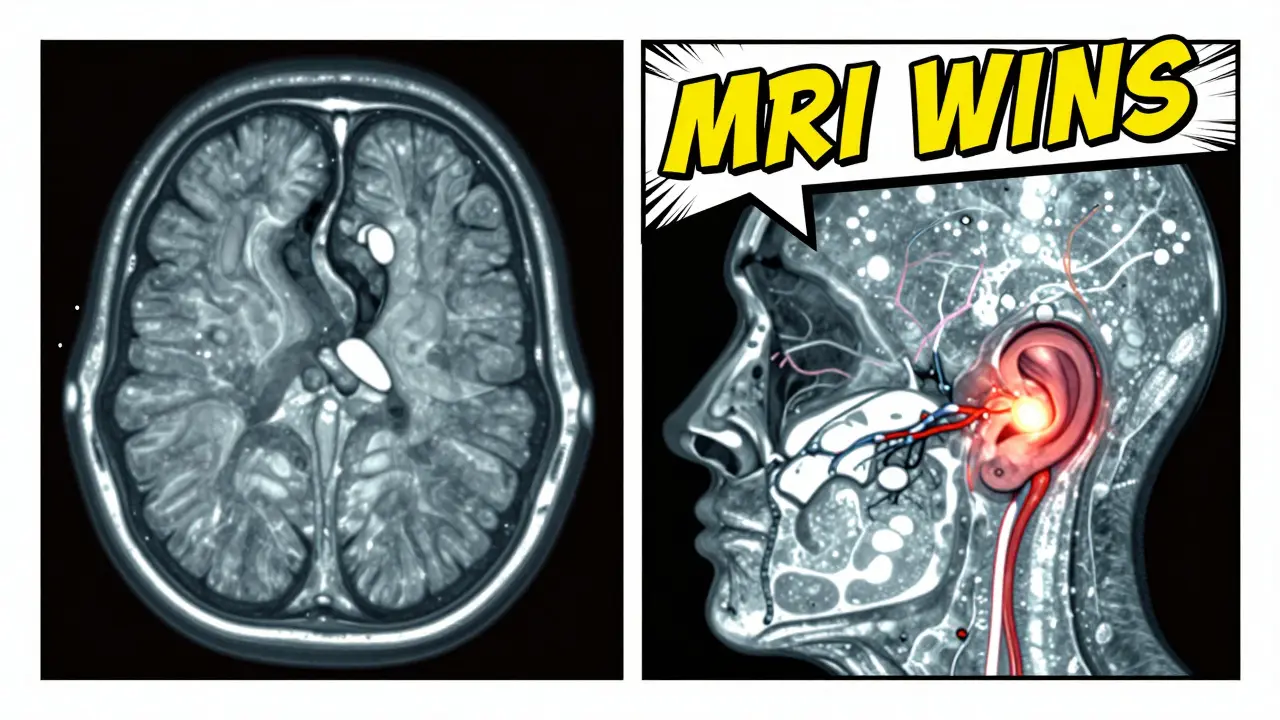
Why MRI Beats CT for Most Neurological Problems
You might wonder why your doctor didn’t just order a CT scan. It’s faster, cheaper, and more available. But for neurological issues, MRI wins in almost every way.CT is great for emergencies-like head trauma or a sudden severe headache where a big bleed is suspected. It can spot a large hemorrhage in under five minutes. But it’s like looking at a black-and-white photo with low resolution. It misses small tumors, early strokes, and inflammation. It also can’t see the back of the brain well because the skull bone blocks the X-rays.
MRIs, on the other hand, give you a full-color, high-definition view. They can detect a 2mm acoustic neuroma-a benign tumor on the hearing nerve-that CT would never catch. They spot early MS plaques with 97% accuracy, while CT misses more than a third. They see small strokes within 30 minutes, while CT might take hours or even days.
And there’s no radiation. That matters if you’re young, pregnant, or need repeat scans over years-like someone with MS or a brain tumor being monitored. MRI can track subtle changes over time. CT can’t.
When MRI Isn’t the Right Choice
MRI isn’t perfect. There are real limits.If you have a pacemaker, certain metal implants, or a cochlear implant, you likely can’t have an MRI. The magnet can move or heat up metal, which is dangerous. Even some tattoos with metallic ink can cause burns. Always tell the technologist about anything metal in your body.
It’s also slow. A brain MRI takes 30 to 45 minutes. If you’re in a car crash, confused, or in severe pain, you might not be able to lie still that long. In those cases, CT is faster and more practical.
And here’s the big one: MRI can’t always tell you how old a lesion is. A bright spot on FLAIR could be a new stroke, an old one, or even a benign cyst. That’s why doctors often need to compare old scans or use contrast dye (gadolinium) to see if there’s active inflammation or a growing tumor. Without contrast, it’s hard to know if something is active or just scar tissue.
There’s also overuse. Studies show that for people with simple migraines and no other neurological symptoms, brain MRIs find abnormalities in only 1.3% of cases. The American College of Radiology says MRI is usually not appropriate for routine headaches without red flags like vision loss, weakness, or sudden onset. Unnecessary scans lead to anxiety, extra tests, and higher costs-without helping.
How Radiologists Read an MRI-Step by Step
You might think reading an MRI is like looking at a photo. It’s not. It’s a systematic process.Experts start in the middle: the ventricles. Are they enlarged? That could mean atrophy or hydrocephalus. Then they check the basal ganglia and thalamus for tiny bright spots-those are lacunar infarcts. Next, they scan the white matter for plaques or small vessel disease. They look at the cortex for signs of stroke or infection. Then they check the brainstem and cerebellum-the areas CT often misses. Finally, they look at the meninges and the spaces around the skull for tumors or inflammation.
One common mistake beginners make? Mistaking a blood vessel for a lesion. Blood vessels have a natural flow void-a black line where blood is moving fast. That’s normal. But if you’re not trained, it can look like a dark hole, which might be mistaken for a hemorrhage or tumor.
Another pitfall? Ignoring the cerebellopontine angle-the space between the brainstem and cerebellum. That’s where small vestibular schwannomas (acoustic neuromas) hide. They’re usually harmless, but if they grow, they can affect hearing or balance. A good radiologist checks this area on every scan.
What’s New in Brain MRI?
MRI isn’t standing still. New tech is making it even more powerful.Ultra-high-field 7.0T MRI machines are now in a handful of academic hospitals. They can show brain layers as thin as 0.5mm-something impossible with standard machines. Researchers use these to study how Alzheimer’s spreads through the brain’s cortex.
Artificial intelligence is cutting scan times in half. Software like Quantib can analyze an MRI in minutes, flagging areas of concern. It doesn’t replace the radiologist-it helps them work faster and catch things they might miss.
Diffusion tensor imaging (DTI) is now used in 68% of MS protocols. It maps the brain’s white matter tracts-the wiring between regions. If those tracts are damaged, DTI shows it, even before the patient has symptoms.
By 2027, quantitative MRI measures like myelin water fraction and cerebral blood flow are expected to become routine. These aren’t just pictures-they’re numbers. They tell you exactly how much myelin (the brain’s insulation) is left, or how much blood is flowing to a tumor. That’s the future: not just seeing the problem, but measuring it.
What to Do After Your MRI
If your MRI shows something abnormal, don’t panic. Many findings are incidental-found by accident and not related to your symptoms.Ask your doctor: Is this new? Is it growing? Does it match my symptoms? Do I need a repeat scan? Will I need contrast next time?
If you’re told you have white matter changes, ask about blood pressure control, cholesterol, and lifestyle. These are modifiable risks. If it’s a small tumor, ask if it’s being monitored or if surgery is needed. If it’s MS, ask about disease-modifying therapies.
And if your scan is normal? That’s good news-but don’t ignore ongoing symptoms. Sometimes the problem isn’t structural. It could be migraine, autoimmune, or even psychological. A normal MRI doesn’t mean there’s nothing wrong. It just means there’s no visible lesion.
Brain MRI is one of the most powerful tools in medicine. But it’s not magic. It’s a map. And like any map, it only helps if you know how to read it-and what questions to ask after you’ve seen it.
Is a brain MRI safe?
Yes, for most people. MRI doesn’t use radiation. But it uses a very strong magnet, so it’s unsafe if you have certain metal implants like pacemakers, cochlear implants, or some aneurysm clips. Always tell the technologist about any metal in your body. Even some tattoos can cause mild burns. The scan is loud, but ear protection is provided. If you’re claustrophobic, ask about open MRI machines or sedation.
How long does a brain MRI take?
A standard brain MRI takes 30 to 45 minutes. High-resolution scans, like those for the inner ear, can take up to an hour. You need to lie very still. Movement blurs the images. If you’re in pain or can’t stay still, let the staff know-they can adjust the position or offer support.
Do I need contrast dye for a brain MRI?
Not always. For many conditions like MS, stroke, or white matter disease, non-contrast MRI is enough. Contrast (gadolinium) is used when doctors suspect active inflammation, infection, or a tumor. It helps show if something is growing or leaking. It’s generally safe, but rare allergic reactions can happen. People with severe kidney disease may not get it due to a small risk of a condition called nephrogenic systemic fibrosis.
Can an MRI detect dementia?
MRI can’t diagnose dementia directly, but it can show patterns that strongly suggest it. For example, shrinkage in the hippocampus (the memory center) is common in Alzheimer’s. Widespread white matter damage points to vascular dementia. MRI also helps rule out other causes like tumors, normal pressure hydrocephalus, or strokes that mimic dementia. It’s one part of the puzzle-along with memory tests and medical history.
Why do I need to compare old MRIs?
A single MRI shows a snapshot. It doesn’t tell you if something is new or has been there for years. Comparing scans helps doctors see if a lesion is growing (which could mean a tumor), shrinking (which might mean treatment is working), or staying the same (which could mean it’s harmless). For conditions like MS, tracking lesion count and size over time is how doctors decide if your treatment needs to change.
If you’ve had a brain MRI, you’re likely trying to understand what’s going on in your body. The images might look confusing, but the patterns aren’t random. With the right context, you can see what’s normal, what’s common with age, and what needs attention. Knowledge turns fear into action-and action leads to better outcomes.

Ashlee Montgomery on 10 January 2026, AT 01:41 AM
It's wild how much detail MRI can show without touching you with radiation. I used to think brain scans were just fancy X-rays until I saw my mom's FLAIR images after her mini-strokes. Those white matter spots looked like constellations. It made me realize how much our brains are silently aging, and how lucky we are to have tools that can see it.
Knowledge really does take the fear out of the unknown.