It’s easy to think that taking more medicine means better results-especially when you’re juggling multiple health issues. But when you’re on five or more medications, the real danger isn’t the number of pills-it’s the hidden duplicates. Many people don’t realize they’re taking the same active ingredient twice, sometimes three times, across prescription and over-the-counter (OTC) drugs. This is called a double ingredient error, and it’s one of the most common and preventable causes of hospitalizations in older adults.
What Exactly Is a Double Ingredient?
A double ingredient happens when you take two or more medications that contain the same active chemical. For example, you might be prescribed Vicodin for pain, which contains acetaminophen, and then pick up a cold medicine like Tylenol Cold & Flu, which also contains acetaminophen. You’re not overdosing on purpose-you just didn’t know both products had the same ingredient. The result? Your liver gets overloaded. The National Institutes of Health reports that more than 56,000 emergency room visits each year in the U.S. are caused by unintentional acetaminophen overdose, and most of them come from this exact scenario.It’s not just acetaminophen. Diphenhydramine, the sleepy-making ingredient in Benadryl, shows up in dozens of OTC sleep aids and cold remedies. Pseudoephedrine, a nasal decongestant, hides in multiple allergy and sinus meds. Even common pain relievers like ibuprofen and naproxen appear in branded and generic versions under different names. If you’re taking multiple prescriptions and OTC products, the chances you’ve accidentally doubled up are higher than you think.
Why This Happens More Often Than You’d Think
The problem isn’t just confusion-it’s systemic. Prescription labels rarely warn you about overlaps with OTC drugs. A 2022 FDA review found that 45% of prescription labels don’t mention that their active ingredients are also in common store-brand medicines. Meanwhile, 68% of people don’t tell their doctors about the herbal supplements, vitamins, or OTC pills they’re taking. That’s a massive blind spot.Older adults are hit hardest. About 40% of Americans over 65 take five or more medications regularly. That’s called polypharmacy. And because they often see multiple specialists-cardiologist, rheumatologist, endocrinologist-each doctor may prescribe something without knowing what the others have ordered. A 2021 study in the Journal of the American Geriatrics Society found that 82% of people who had a double ingredient incident had visited more than three doctors in the past six months. And in two out of three cases, none of those providers ever asked about their OTC meds.
Even the labels on OTC products aren’t foolproof. The FDA required standardized “Drug Facts” labels in 2020 to make ingredients clearer. But a 2023 Government Accountability Office report found that 41% of people still can’t spot duplicate ingredients on those labels. One patient told UCLA Health, “I didn’t realize my prescription painkiller and the store-brand cold medicine had the same thing in them-until I ended up in the ER with liver damage.”
Who’s Most at Risk?
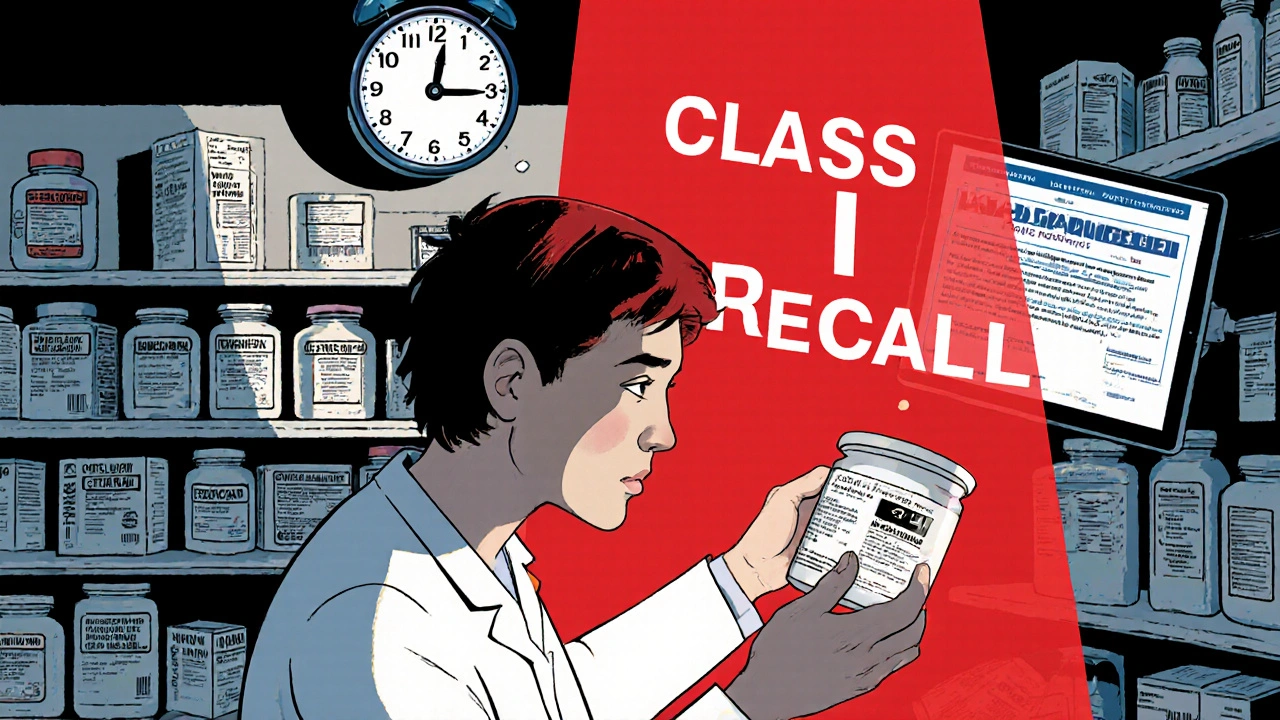
If you’re over 65, taking five or more medications, or seeing multiple doctors, you’re in the highest-risk group. The CDC says adults 65 and older account for 65% of hospitalizations due to double ingredient errors. But it’s not just age-it’s complexity. People with three or more chronic conditions (like diabetes, heart disease, and arthritis) are far more likely to be on multiple drugs. And since multimorbidity has gone up 27% since 2010, this problem is growing.People who shop at multiple pharmacies are also at higher risk. When you fill prescriptions at different stores, the pharmacy’s safety system can’t see everything you’re taking. A 2021 JAMA Internal Medicine study showed that using just one pharmacy cuts double ingredient errors by 63%. That’s because single pharmacies use software that flags interactions across all your prescriptions-and even some OTCs if you buy them there.
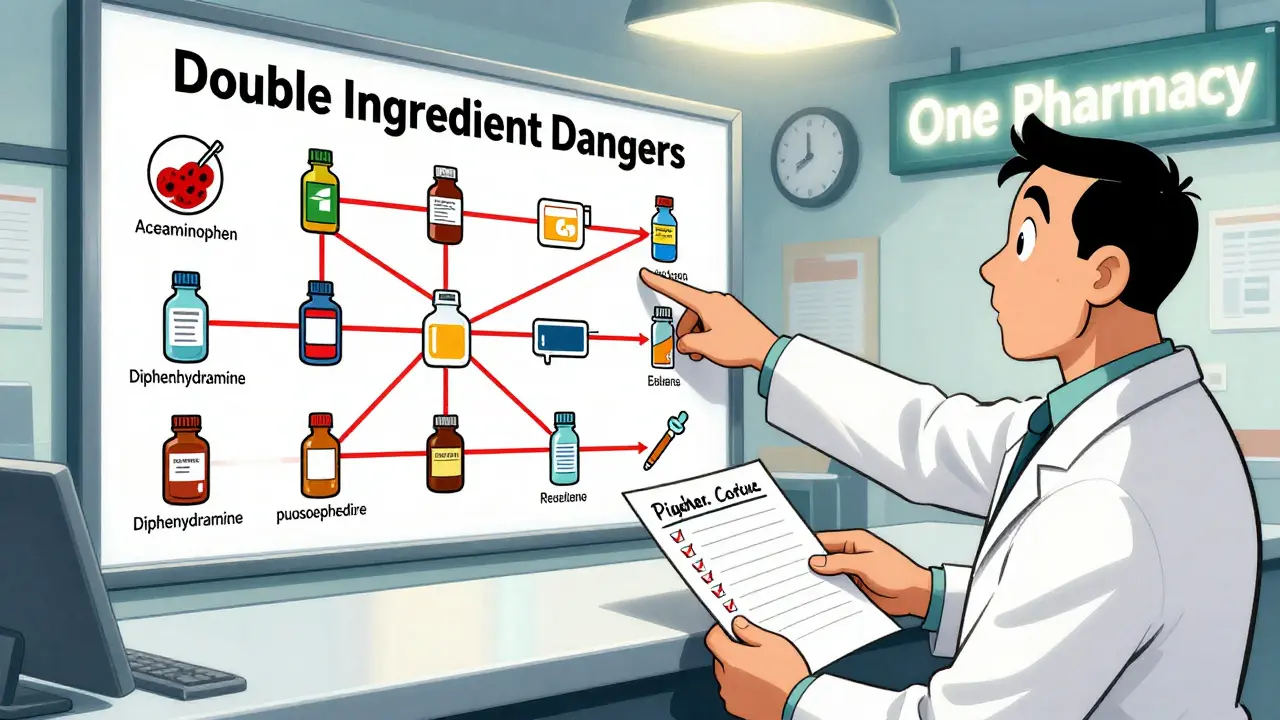
Common Culprits: The Top 5 Double Ingredient Traps
Here are the most frequent offenders that catch people off guard:- Acetaminophen (Tylenol, Panadol): Found in over 600 OTC and prescription products, including Vicodin, Percocet, Excedrin, and many cold and flu formulas.
- Diphenhydramine (Benadryl): Appears in sleep aids like Unisom, allergy meds like NyQuil, and even some motion sickness pills.
- Pseudoephedrine: Used in Sudafed, Claritin-D, and many “sinus” or “congestion” relief products.
- NSAIDs (ibuprofen, naproxen): Found in Advil, Aleve, and also in some combination cold and arthritis meds.
- Anticholinergics (like oxybutynin, chlorpheniramine): Used for overactive bladder, allergies, and motion sickness. Often hidden in OTC products labeled “for nighttime relief.”
The American Geriatrics Society’s Beers Criteria®-updated in 2023-now lists 15 high-risk double ingredient combinations involving these substances. If you’re taking any of these, you need to check your full list.
How to Protect Yourself: 5 Action Steps
You don’t need to be a pharmacist to avoid these errors. Here’s what actually works:- Make a full medication list-every single one. Write down the name, dose, how often you take it, and why you’re taking it. Include prescription drugs, OTC pills, vitamins, herbal supplements, and even topical creams if they contain active ingredients. Keep a copy in your wallet and another at home. This is the single most effective step. Studies show it reduces double ingredient errors by 78%.
- Fill all prescriptions at one pharmacy. This gives your pharmacist a complete view of your meds. Community pharmacists catch double ingredient issues in 87% of medication therapy consultations, according to Pharmacy Times. They’re trained to spot these, and they’re often the last line of defense.
- Ask your doctor or pharmacist: “Could this interact with anything else I’m taking?” Don’t wait for them to ask. Bring your list to every appointment-even if it’s for a cold. Say, “I’m taking these. Is anything here a duplicate?”
- Read OTC labels like a detective. Look for the “Active Ingredients” section. Don’t just read the brand name. If you see acetaminophen, diphenhydramine, or ibuprofen on your prescription and again on your cold medicine, stop and call your pharmacist before taking both.
- Review your meds once a year. Schedule a “medication check-up” with your primary care provider. Bring your full list. Ask: “Are all these still necessary? Are any of them overlapping?” This simple step can cut your risk by more than half.

Technology Is Helping-But It’s Not Perfect
Electronic health records now have “double ingredient check” tools built in. Epic and Cerner, the two biggest systems used in U.S. hospitals, alert providers when a new prescription matches an existing one. That works well for prescriptions-but only if the OTC meds are entered. And they rarely are. A 2022 KLAS report found that only 43% of EHR systems track OTC use properly.Some new tools are making a difference. Apple Health, since iOS 17 (released in 2023), now flags duplicate active ingredients if you manually enter your meds. Tabula Rasa HealthCare’s MedWise Risk Score uses AI to analyze your full list and gives you a risk rating with 89% accuracy. But these tools only work if you use them. You still have to enter your OTC meds manually.
What to Do If You’ve Already Had a Problem
If you’ve ever felt dizzy, nauseous, overly sleepy, or had stomach pain after starting a new OTC med while on prescriptions, you might have had a double ingredient reaction. Don’t ignore it. Go to your pharmacist or doctor with your full medication list. Say: “I think I might have taken too much of the same thing.”One Reddit user, “MedSafety101,” shared a story that got over 2,300 upvotes: They took three different cold meds-all containing pseudoephedrine-and ended up in the ER with dangerously high blood pressure. “I thought I was just being careful,” they wrote. “I didn’t know each one had the same active ingredient.”
That’s the tragedy. It’s not negligence. It’s lack of information.
Bottom Line: You’re Not Alone, But You’re Not Powerless
Double ingredient errors are common, preventable, and often invisible. They’re not caused by being careless-they’re caused by a system that doesn’t connect the dots between your prescriptions, your OTC meds, and your supplements.But you have control. Start today. Make your list. Fill at one pharmacy. Ask the questions. Read the labels. You don’t need to remember every chemical name. You just need to know: “Is this the same thing as something else I’m already taking?”
The goal isn’t to stop taking your meds. It’s to take them safely. One pill too many of the same ingredient can send you to the hospital. One simple list can keep you out.
What’s the most common double ingredient mistake?
The most common mistake is combining prescription painkillers like Vicodin or Percocet with OTC cold and flu medicines like Tylenol Cold or NyQuil. Both contain acetaminophen, and taking them together can cause severe liver damage. Over 56,000 emergency room visits each year in the U.S. are due to this exact error.
Can I trust OTC labels to tell me if I’m doubling up?
OTC labels now follow FDA’s “Drug Facts” format, which lists active ingredients clearly. But studies show 41% of people still can’t identify duplicate ingredients from these labels. Always compare the active ingredient list on your prescription with what’s on the OTC bottle. Don’t rely on brand names-look for the chemical names like acetaminophen, diphenhydramine, or ibuprofen.
Should I stop taking OTC meds if I’m on multiple prescriptions?
No-don’t stop anything without talking to your doctor or pharmacist. But do review every OTC product you take. Many people use them daily for headaches, sleep, or allergies without realizing they’re adding to their prescription load. Bring your full list to your next appointment and ask: “Is this still safe with everything else I’m taking?”
Why do doctors often miss these double ingredient issues?
Most doctors focus on one condition at a time, and they rarely ask about OTC meds, supplements, or herbal products. Only 33% of providers routinely ask patients about non-prescription drugs. Also, electronic health records rarely include OTC use unless the patient enters it. That means your doctor may not even know you’re taking Advil every day for arthritis while they’ve prescribed you a different NSAID.
How often should I review my medications?
At least once a year, but better yet-every time you start a new medication or see a new doctor. A 2021 study in the Annals of Internal Medicine showed that when providers checked medication lists against patient diagnoses, double ingredient errors dropped by 54%. Make it a habit: bring your list to every appointment, no matter how small the reason.
Is it safe to use a medication app to track my pills?
Yes-if the app lets you enter both prescription and OTC medications. Apps like Apple Health, Medisafe, or MyTherapy can help you track doses and flag duplicates. But they only work if you enter everything. Don’t just add prescriptions-add your daily aspirin, sleep aids, antacids, and vitamins. The more complete your list, the better the app can protect you.



Paula Villete on 23 December 2025, AT 14:34 PM
I swear, I took three different cold meds last winter and woke up feeling like my liver had filed a complaint against me. Turns out, every single one had acetaminophen. I didn't even know it was in the 'nighttime relief' stuff. Now I keep a printed list in my wallet. My pharmacist calls it 'the holy grail of safety.' I call it my survival guide.
Also, if you're using 'natural' sleep aids, check the label. Melatonin doesn't cause liver damage, but diphenhydramine does. And yes, that's in your 'herbal' tea too. Don't trust the word 'natural'-trust the chemical name.