Medication Review Prep Checklist
Prepare for Your Telehealth Medication Review
This checklist ensures you're ready for your telehealth medication review. Studies show patients who display their medications during the call increase review accuracy by 37.4%.
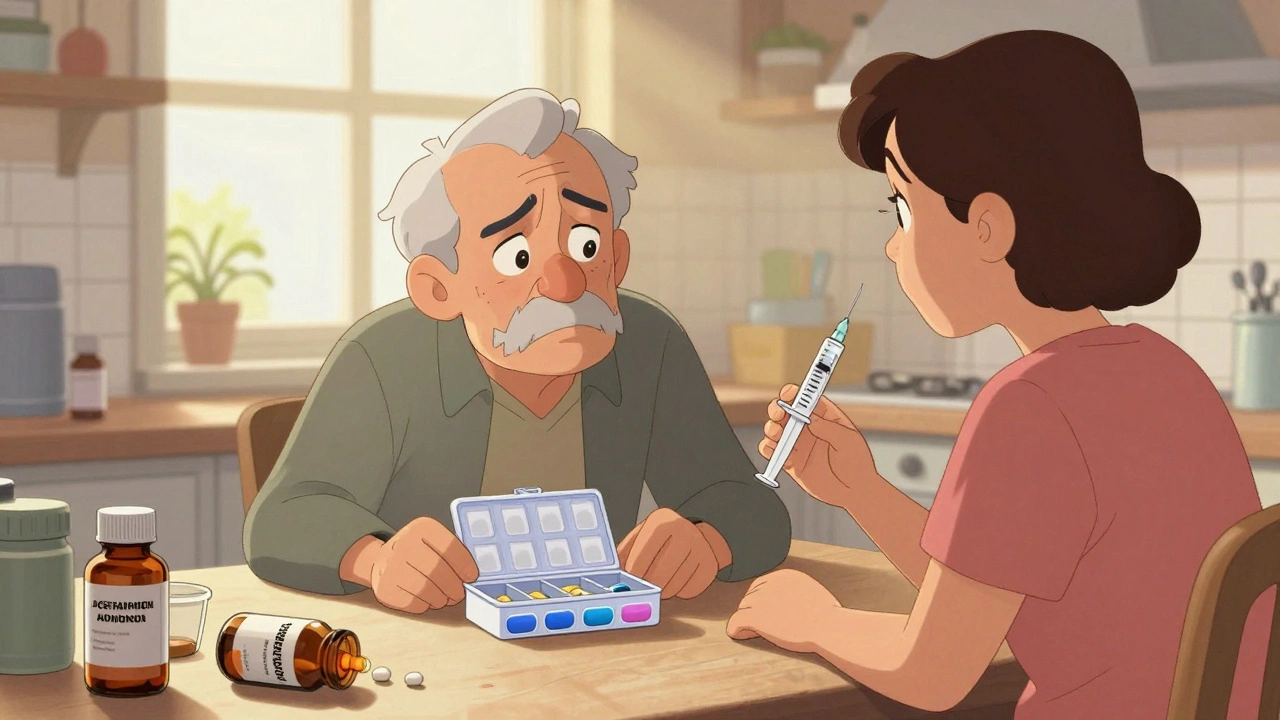
When you’re managing multiple medications-prescriptions, over-the-counter pills, vitamins, or supplements-mistakes happen. A pill taken at the wrong time, a dangerous interaction between drugs, or a side effect missed because no one asked the right question. That’s where a telehealth medication review comes in. It’s not just a video call with your pharmacist. It’s a safety check designed to catch errors before they hurt you. And if you’re preparing for one, knowing exactly what to do and what to ask can make all the difference.
Why Telehealth Medication Reviews Matter Now
More than 78% of U.S. healthcare systems now offer telehealth medication reviews. That’s not a trend-it’s a necessity. With an aging population, more people taking five or more medications daily, and pharmacy errors contributing to over 1.5 million preventable injuries each year, these reviews are a lifeline. A 2020 study found elderly patients who got virtual medication reviews had 34.7% fewer dangerous drug reactions than those who didn’t. That’s not a small number. It’s lives saved.
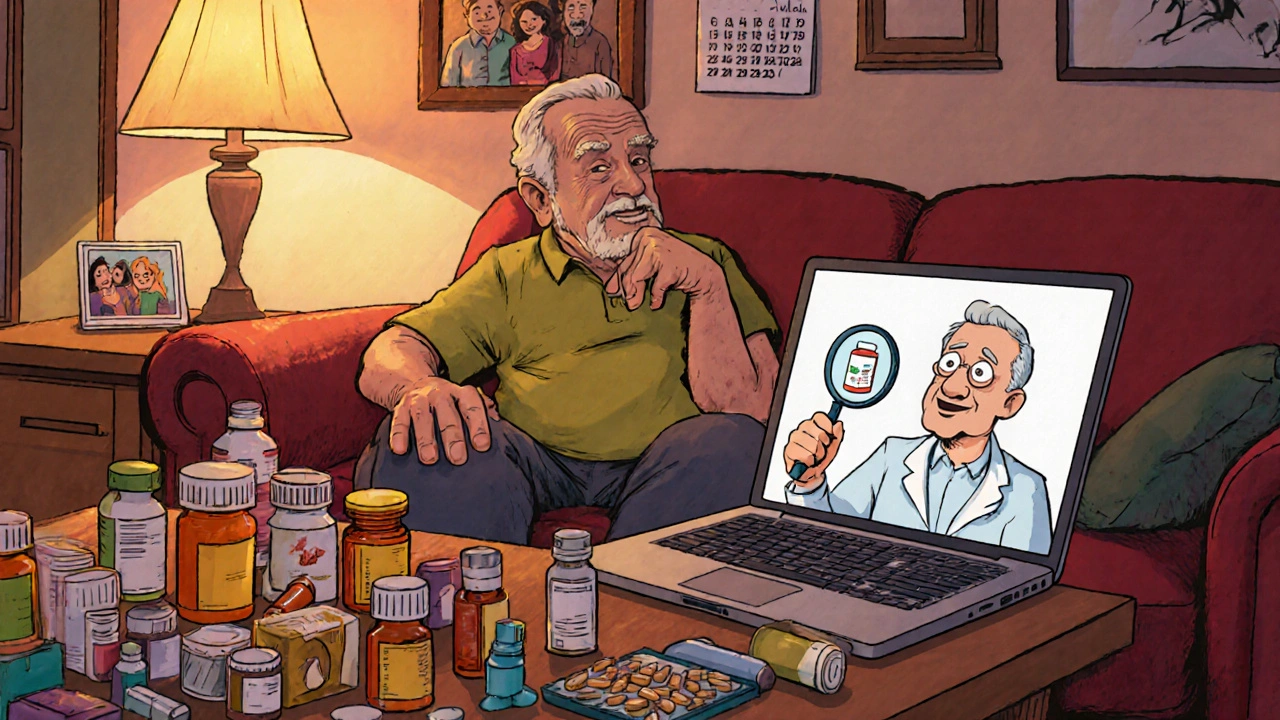
Unlike in-person visits, telehealth reviews happen in your living room. No traffic, no waiting room, no rushing between appointments. But that convenience comes with a catch: you have to be ready. If you just show up and hope the pharmacist figures it out, you’re leaving safety to chance.
What You Need to Gather Before Your Call
Before your video appointment, gather everything you take. Not just what’s in your medicine cabinet. Everything.
- All prescription bottles-even ones you haven’t used in months
- Over-the-counter meds: painkillers, sleep aids, antacids
- Vitamins, supplements, herbal remedies
- Any creams, patches, or inhalers you use
Put them all in a clear bag or on a table where the camera can see them. A 2023 study showed patients who displayed their actual medications during the call increased review accuracy by 37.4%. Why? Because people forget. They think, “Oh, I haven’t taken that in a while,” but the pharmacist needs to know it’s still in your house. That’s how dangerous interactions slip through.
Also, have a written list ready. Write down:
- What each pill is for
- When and how often you take it
- Any side effects you’ve noticed
- Whether you’ve skipped doses or changed how you take them
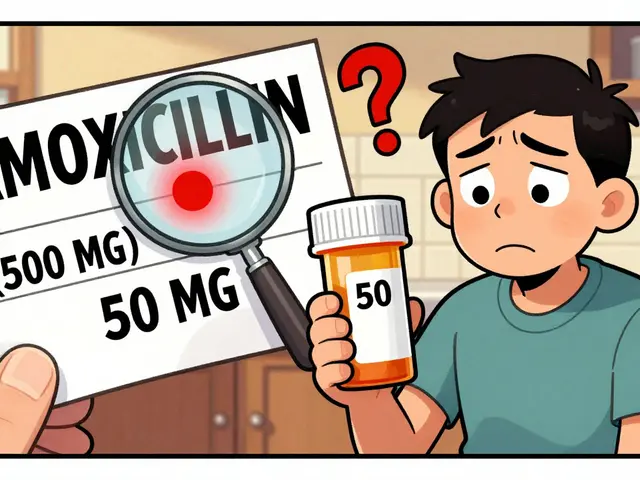
Don’t rely on memory. If you’re unsure about a pill, take a photo of the label. That’s better than guessing.
What to Ask During the Review
Most patients sit quietly during these calls. Don’t. This is your safety check. You have the right-and the responsibility-to ask questions. Here are the five most important ones:
- “How will you verify my medication list against my pharmacy records?”
Forty-three percent of medication errors come from inaccurate lists. Your pharmacist might not have access to every pharmacy you’ve used. If they’re just going by what you say, they’re flying blind. Ask them to cross-check with your electronic records. If they say they can’t, push for a follow-up with your primary care provider. - “What is your process for communicating recommendations to my doctor?”
Only 62.8% of telehealth services have a standardized way to send changes to your GP. If the pharmacist says, “I’ll just let them know,” ask how. Do they email? Fax? Call? Get a copy of the report they send. You deserve to know what’s being recommended. - “Are any of these medications no longer needed?”
Many people keep taking pills long after they’re useful. Blood pressure meds after a successful surgery? Cholesterol drugs after switching diets? Ask if anything can be safely stopped. Reducing unnecessary pills lowers your risk of side effects and saves money. - “How will you monitor for side effects between appointments?”
Virtual reviews can miss signs of trouble. A rash, dizziness, or confusion might not show up on camera. Ask if they’ll schedule a follow-up call, send a text check-in, or coordinate with your doctor for lab tests. Without this, you’re on your own if something goes wrong. - “Are there any dangerous interactions I should watch for?”
Don’t let them assume you know. Say it plainly: “I’ve heard some of these can clash. Can you walk me through what to look out for?” Common risky combos include blood thinners with NSAIDs, antidepressants with sleep aids, or statins with grapefruit juice. Don’t be shy-this is why you’re here.
What Telehealth Can’t Do (And When You Still Need an In-Person Visit)
Telehealth is powerful-but it’s not magic. It works best for stable, chronic conditions: high blood pressure, diabetes, thyroid meds, depression. But it falls short in some areas.
If you have:
- Multiple chronic illnesses with complex symptoms
- Signs of confusion, memory loss, or sudden weakness
- Difficulty swallowing pills or using inhalers
- Unexplained weight loss or falls
-then you need a face-to-face check. A 2021 study found telehealth reviews missed critical issues in 17.3% of patients with multiple conditions because they couldn’t examine physical signs like swollen ankles, tremors, or skin changes.
Also, if you’re taking Schedule II controlled substances (like oxycodone or Adderall), federal rules require an in-person visit at least once every three months. The DEA’s 2025 rules allow telehealth for other controlled substances, but not these. Know your meds’ schedule.
Common Problems and How to Fix Them
Technical issues are the #1 complaint. Video freezes, poor audio, apps that won’t open. Here’s how to avoid them:
- Test your camera and mic 15 minutes before the call
- Use Wi-Fi, not mobile data-minimum 1.5 Mbps upload speed
- Close other tabs and apps during the call
- Have a backup phone ready in case your computer fails
Another issue? Time. Many reviews are rushed. If the pharmacist cuts you off after 10 minutes, say, “I have more to discuss-can we schedule a follow-up?” You’re not being difficult. You’re being smart.
And if you’re over 65? You’re not alone if tech feels overwhelming. A 2024 survey found seniors who got 15-minute tech training before their review were 68% more comfortable than those who didn’t. Ask your provider if they offer a practice call. Many do.

What Happens After the Review?
The review doesn’t end when the video ends. You should get a written summary within 48 hours. It should list:
- Changes to your meds
- Medications to stop
- New prescriptions or dosages
- Next steps and follow-up timeline
Keep this document. Share it with your primary care doctor. If you don’t get it, call and ask. No summary means no accountability.
Also, watch for changes in how you feel over the next two weeks. Did your sleep improve? Did your dizziness get worse? Note it down. That feedback helps your pharmacist adjust your plan.
Final Thought: This Is Your Health, Not Just a Check-In
A telehealth medication review isn’t a formality. It’s a critical safety net. You’re not just handing over a list-you’re protecting yourself from harm. The system works best when you’re involved. Show up prepared. Ask the hard questions. Don’t let convenience make you passive.
Medication errors don’t always cause crashes. Sometimes, they just make you feel worse-tired, foggy, achy. And you might think that’s just aging. It’s not. It could be a drug interaction. A telehealth review can find it. But only if you’re ready to speak up.
Do I need to have all my medications in front of me during the telehealth review?
Yes. Studies show that patients who physically display their medications during the call improve review accuracy by 37.4%. Pharmacists can’t guess what you’re taking. Seeing the actual bottles or labels helps them spot duplicates, expired drugs, or incorrect dosages. If you can’t get all bottles out, take clear photos of each label and have them ready to share on screen.
Can a pharmacist change my prescription during a telehealth review?
No, they can’t prescribe or change your dosage directly. But they can recommend changes to your doctor. If they suggest stopping a medication, switching doses, or adding a new one, they’ll send a formal note to your GP or specialist. You should receive a copy of that recommendation. Always follow up with your doctor to confirm the changes were made.
Are telehealth medication reviews covered by insurance?
Yes, if you’re on Medicare or many private plans. As of November 2024, Medicare covers two new codes: G2225 for comprehensive reviews ($142.37) and G2226 for targeted reviews ($78.92). Most private insurers follow suit. Check with your plan, but if you’re on a chronic condition management program, you’re likely eligible. Don’t assume it’s out-of-pocket-ask.
What if I’m not comfortable using video technology?
Many providers offer phone-only reviews if video isn’t possible. However, video is strongly preferred because pharmacists need to see your medications and observe signs like tremors or confusion. If you struggle with tech, ask if your provider offers a practice call or a family member can help set up the session. Some community centers even offer free tech support for seniors before appointments.
How often should I have a telehealth medication review?
At least once a year if you’re taking three or more medications regularly. If you’ve recently been hospitalized, had a major health change, or started new drugs, get a review within 30 days. People who get reviews after hospital discharge reduce their risk of 30-day readmission by 22.1%. Don’t wait for problems-schedule it proactively.



Diane Tomaszewski on 15 November 2025, AT 05:31 AM
It's funny how we treat meds like they're magic bullets instead of tools. You wouldn't drive a car without checking the oil, but we take ten pills a day and never ask why. This post gets it right-you gotta be the one holding the flashlight in the dark.