Every time you pick up a prescription, there’s a small sticker on the bottle. It might say take with food, do not crush, or black box warning. You’ve probably glanced at it, maybe read it once, and then tossed the paper insert. But those stickers? They’re not just bureaucracy. They’re your last line of defense against a dangerous mistake.
What Those Stickers Are Really For
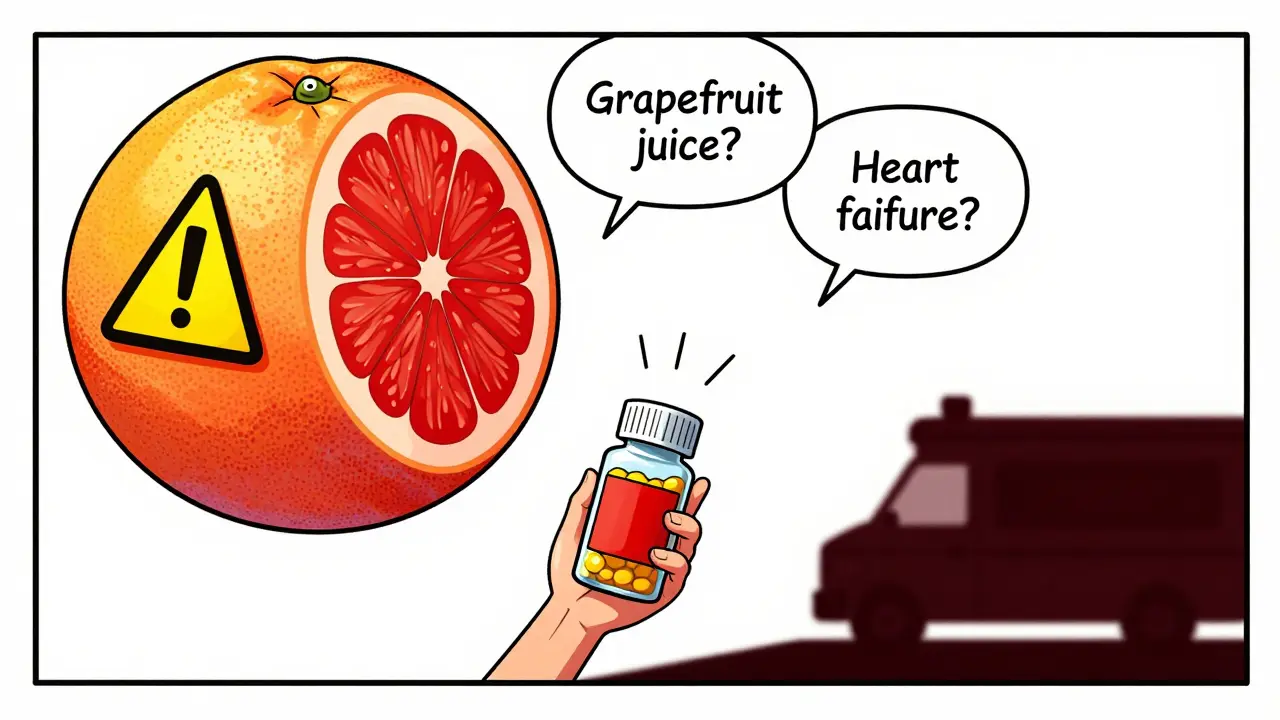
Those little labels aren’t random. They’re legally required by the FDA to stop you from getting hurt. The U.S. Food and Drug Administration mandates that every prescription container carries warnings that are clear enough to prevent injury. And it’s not just about side effects-it’s about how you take the medicine, what you can’t mix it with, and when you absolutely must not take it at all.Think of it like this: your doctor prescribes the right drug. The pharmacist fills it correctly. But if you swallow a pill you were told not to crush, or drink grapefruit juice with your blood pressure med, the whole chain breaks. That’s where the sticker steps in. It’s the final safety check before the medicine hits your body.
According to the Institute of Medicine, medication errors cause about 1.3 million injuries and 7,000 deaths every year in the U.S. A big chunk of those? They happen because patients didn’t understand the warning labels.
Black Box Warnings: The Red Flag You Can’t Ignore
Not all warnings are created equal. The most serious ones are called Black Box Warnings. These aren’t stickers-they’re bold, boxed statements printed right on the drug’s official prescribing info, and they’re copied onto the label when the risk is life-threatening.These warnings are reserved for drugs that can cause death or severe injury. Think heart failure, liver damage, suicidal thoughts, or dangerous interactions. About 40% of new drugs approved between 2013 and 2017 carried one. If your pill has this warning, it doesn’t mean don’t take it. It means: pay attention.
For example, some antidepressants carry a Black Box Warning about increased suicide risk in young adults under 25. That doesn’t mean you shouldn’t take them. It means you and your doctor need to watch closely in the first few weeks. If you see sudden mood swings, withdrawal, or talk of self-harm, call your doctor immediately. The sticker isn’t scaring you-it’s telling you what to watch for.
Color-Coded Warnings: Red Means Stop, Yellow Means Slow Down
You’ve seen them: red stickers, yellow ones, sometimes blue or green. Colors aren’t random. A 2017 study in U.S. Pharmacist found that patients naturally read color as a signal of danger.Red? That’s a red flag. It means immediate risk: severe allergic reaction, dangerous interaction, or life-threatening side effect. Yellow means caution: possible drowsiness, risk of falls, or something you need to monitor. Blue, white, or green? Those are usually reminders-like take with food or refrigerate-not emergencies.
But here’s the catch: not every pharmacy uses color consistently. Some still print everything in black. So don’t rely on color alone. Read the words. If you see Do not operate heavy machinery, that’s not a suggestion. That’s a warning you could pass out behind the wheel.
What “Take with Food” Really Means
You’ve probably heard this one: Take with food. Sounds simple, right? But 42% of people who ignored it ended up with nausea, vomiting, or worse.“Take with food” doesn’t mean “have a snack later.” It means: take the pill during or right after a meal. Why? Some drugs irritate your stomach lining if taken empty. Others won’t absorb properly without fat or protein. For example, the antibiotic doxycycline can cause severe heartburn if taken on an empty stomach. But if you take it with a big glass of water and a sandwich, it’s fine.
Same goes for take on an empty stomach. That means at least one hour before eating or two hours after. If you pop your thyroid med with your morning coffee and toast, you’re not getting the full dose. Your body just can’t absorb it right.
Why “Swallow Whole” Is a Lifesaver
Another common one: Do not crush, chew, or break. Patients misunderstand this all the time. Some think it means “chew it up so it works faster.” Others crush pills to mix them in applesauce because they can’t swallow pills.But crushing a time-release pill? That’s like setting off a bomb. Those pills are designed to slowly release medicine over 8, 12, or even 24 hours. Crush it, and you get the full dose all at once. That can cause overdose-even with drugs you’ve taken safely before.
One 2022 Reddit thread from pharmacists showed 30% of patients misread this warning. A man crushed his extended-release oxycodone because he couldn’t swallow it. He ended up in the ER with respiratory failure. The sticker wasn’t optional. It was a life-or-death instruction.
Why You Should Never Trust the Paper Insert
That big booklet that comes with your prescription? Most people throw it away. And that’s a problem.A 2020 study found that 68% of patients toss the Patient Prescribing Information (PPI) sheet-right after they get home. But that’s where the real details live: drug interactions, what to do if you miss a dose, signs of a bad reaction.
One patient on Drugs.com shared how she threw away the paper warning about grapefruit juice and her blood pressure med. Two days later, she ended up in the ER with dangerously low blood pressure. The sticker on the bottle said “avoid grapefruit,” but she didn’t see it. The insert had the full warning. She never read it.
Don’t rely on the sticker alone. Keep the insert. Or better yet-ask your pharmacist to explain it to you. Most will do it for free.

What to Do When You Don’t Understand
You’re not dumb if you don’t get it. The FDA admits that 80 million American adults have trouble understanding medical info. That’s not your fault. It’s the system’s failure.Here’s what works:
- Ask the pharmacist to explain it in your own words. Say: “Can you tell me what this means in plain English?”
- Use the teach-back method. After they explain, say: “So if I take this with grapefruit, I could get dizzy and pass out-is that right?” If they say yes, you got it.
- Check for QR codes. Starting in 2024, some pharmacies are putting QR codes on labels. Scan it with your phone, and you’ll get a short video explaining the warning.
- Write it down. If the warning says “avoid sunlight,” write “Wear hat and sunscreen when outside” on your phone or a sticky note.
Pharmacies like Walgreens that use their “Medication Safety Check” program have 92% patient comprehension. Independent pharmacies without structured counseling? Only 68%. Don’t assume you’ll get the help you need-ask for it.
What’s Changing in 2025 and Beyond
The system is finally waking up. In 2022, the FDA launched the “Facts Label” initiative. By June 2025, 20 high-risk drug classes-including blood thinners, diabetes meds, and heart drugs-must use simplified, easy-to-read labels with icons and plain language.They’re also rolling out universal symbols. A new “do not crush” icon? It used to be misread 31% of the time. Now? Only 8%. That’s a huge win.
By 2026, most pharmacies will be required to use these new standards. But until then? You still have to be your own advocate.
Bottom Line: Your Stickers Are Your Safety Net
Prescription labels aren’t meant to confuse you. They’re meant to protect you. But they only work if you read them, understand them, and act on them.Don’t assume you know what take with food means. Don’t ignore a red sticker because you’ve taken the pill before. Don’t crush a pill because it’s hard to swallow. And don’t throw away the paper insert.
If you’re unsure? Ask. Always. Your pharmacist is there to help-not to judge. And if they don’t explain it clearly, go somewhere else. There’s no shame in asking. There’s only danger in staying silent.
Medication errors aren’t accidents. They’re preventable. And the next time you pick up a bottle, take two seconds to read the sticker. It might just save your life.




Mike Rose on 1 February 2026, AT 08:34 AM
lol who even reads these stickers? i just swallow the pill and hope for the best. my grandma died from a med error but she was old so like... whatever.