It happens to everyone. You walk out of the pharmacy with a new prescription, open the bottle, and stare at the label. Take one by mouth twice daily - but what does that really mean? Twice a day, but when? With food? Can you take it if you miss a dose? And why does this bottle say something different than the last one you had?
Confusing medication instructions aren’t just annoying. They’re dangerous. In the U.S., unclear directions contribute to more than 1.5 million medication-related injuries every year, according to the Institute for Safe Medication Practices. These aren’t rare mistakes. They’re everyday risks, especially when people are taking three or more drugs. If you’ve ever felt unsure about how to take your medicine, you’re not alone - and you’re not being difficult. The system is messy.
Why Medication Instructions Are So Hard to Understand
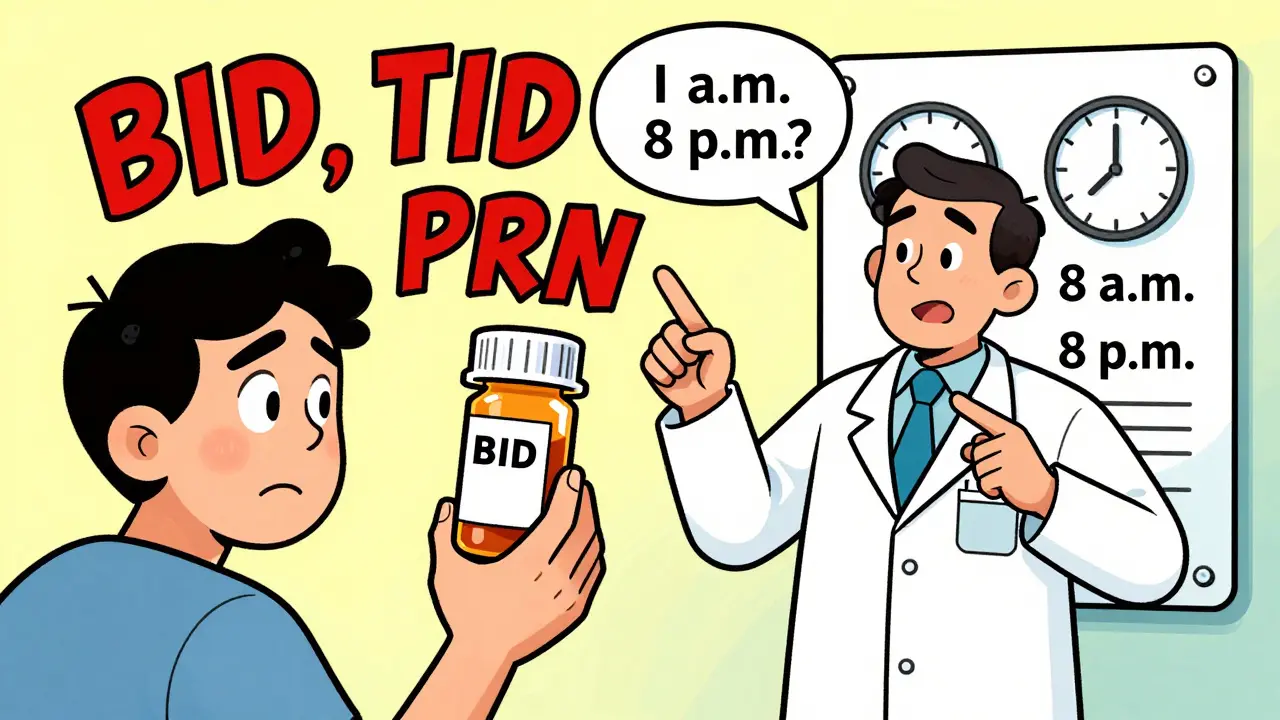
Prescription labels often use shorthand that makes sense to doctors and pharmacists - but not to patients. Things like "q.d." for daily, "BID" for twice a day, or "PO" for by mouth are common in medical charts. But they’re not meant for public use. The FDA and the Institute for Safe Medication Practices (ISMP) have been pushing for years to stop these abbreviations. Instead, they want plain language: "take once daily," "take by mouth," "take with food."
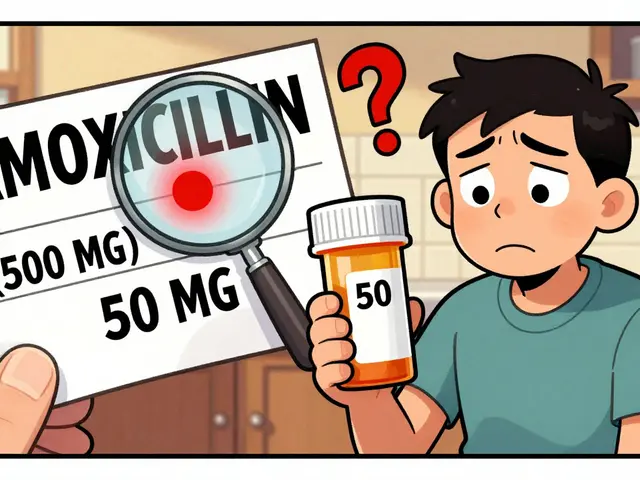
Even when instructions are written clearly, problems still arise. Different manufacturers of the same drug - say, generic metformin - might list slightly different dosing advice. One says "take with meals," another says "take 30 minutes before meals." Which one is right? The National Institutes of Health says clinicians should check both and explain the differences to patients. But in practice, that rarely happens unless you ask.
Timing matters too. Some medications work best at night because your body produces more of the substance they’re trying to block - like cholesterol. Others need to be spaced evenly, like every 12 hours, to keep a steady level in your blood. If you take a pill at 8 a.m. and then again at 10 p.m., you’re not getting the full benefit. And if you take a painkiller "as needed," how much is too much? How often? These details aren’t always on the label.
What You Should Do When Instructions Don’t Make Sense
Don’t guess. Don’t assume. Don’t wait until you feel worse. Ask - clearly and directly.
- Call your pharmacist. Pharmacists are medication experts. They see dozens of patients every day who are confused about the same thing. They can explain what "BID" means, how to space doses, and whether it’s safe to take with coffee or grapefruit juice.
- Ask your doctor or nurse. If the instructions conflict with your previous prescription, or if you’re switching brands, say: "I noticed the directions changed. Can you help me understand why?" This isn’t a dumb question - it’s smart.
- Request a Medication Guide. For high-risk drugs like opioids, isotretinoin, or blood thinners, the FDA requires pharmacies to give you a printed guide. It explains risks, side effects, and exactly how to take the drug. If you didn’t get one, ask for it. You’re entitled to it.
- Use a pill organizer with labels. Write down the time, dose, and purpose for each pill. If you’re taking something at bedtime, write "Cholesterol med - take at 10 p.m." on the compartment. Visual cues reduce errors.
- Set phone reminders. The CDC recommends this for anyone taking multiple medications. Set two alarms: one for morning, one for night. Add a note: "Take with breakfast," or "Don’t take if you’re dizzy."
What Pharmacists Are Required to Tell You
In outpatient settings - like your local pharmacy - pharmacists must give you a Medication Guide if your drug is on the FDA’s list of high-risk medications. That list includes over 200 drugs as of 2023. These guides are not optional. They’re legally required.
But here’s the catch: Medication Guides are only required for certain drugs. For most others - like antibiotics, blood pressure pills, or thyroid meds - there’s no printed guide. That doesn’t mean you shouldn’t get clear instructions. Pharmacists are still expected to counsel you on how to take the drug, what side effects to watch for, and what to do if you miss a dose. If they don’t offer it, ask: "Can you walk me through how to take this?"
Some pharmacies offer digital versions of Medication Guides you can access on your phone. If you prefer that, say so. You have the right to choose how you receive the information - paper or digital.
What Hospitals and Nursing Homes Do Differently
In hospitals or long-term care facilities, you won’t get a printed Medication Guide. Instead, nurses and doctors are required to explain the medication to you or your caregiver before giving it. That includes telling you:
- What the drug is for
- How to take it
- What side effects to expect
- What to do if you feel unwell
But this doesn’t always happen. Staff are busy. Patients are tired. If you’re in the hospital and no one explains your meds, say: "I don’t know why I’m taking this. Can you tell me?" It’s your right. If you’re helping a loved one, ask the same questions - even if they seem obvious.
One common mistake: assuming a new pill is the same as an old one. Two different brands of the same drug can have different fillers, release rates, or dosing instructions. Always compare the new bottle to the old one. If something looks different - color, shape, size, or label - ask before taking it.
Real Examples of Confusing Instructions - and How to Fix Them
Here are real-world cases that show how small wording changes can make a big difference:
- Old label: "Take 1 tab PO q.d." → Fix: "Take one tablet by mouth once daily."
- Old label: "Take as needed for pain." → Fix: "Take one tablet for pain, up to three times a day. Wait at least 6 hours between doses. Do not take more than three tablets in 24 hours."
- Old label: "Take 500 mg bid." → Fix: "Take 500 milligrams twice a day, about 12 hours apart - for example, at 8 a.m. and 8 p.m."
- Old label: "Take on an empty stomach." → Fix: "Take at least one hour before eating, or two hours after a meal."
These aren’t just improvements - they’re safety steps. The ISMP has a list of 15 banned abbreviations. "q.d." is one. "BID" is another. "IN" for intranasal is dangerous because it looks like "IV." Always write it out.

What to Do If You Can’t Reach Your Doctor
Sometimes, you need help right away - but your doctor’s office is closed. That’s when your pharmacist becomes your best ally. Most pharmacies have a clinical pharmacist on staff or on-call after hours. Call them. They can:
- Clarify dosing
- Check for interactions with other meds you’re taking
- Advise if it’s safe to wait until morning
- Help you get a new prescription if the instructions are wrong
Don’t wait until you feel sick to ask. If you’re unsure, assume the worst-case scenario: taking it wrong could cause harm. Better to call and look overcautious than to risk an adverse reaction.
How to Keep Track of All Your Medications
If you take multiple drugs, write them down. Keep a list that includes:
- Drug name (brand and generic)
- Dose (e.g., 10 mg)
- How often (e.g., once daily)
- When to take it (e.g., with breakfast, at bedtime)
- Purpose (e.g., "for blood pressure," "for cholesterol")
- Prescribing doctor
Update it every time you get a new prescription. Bring it to every appointment. Show it to your pharmacist. This simple habit prevents dangerous overlaps and missed clarifications.
Apps like MyTherapy, Medisafe, or even your phone’s notes app can help. But don’t rely on memory. Write it down. Even if it’s on a napkin. Then keep it in your wallet.
Final Rule: If You’re Unsure, Ask - No Matter Who You’re Talking To
Harvard Health says it plainly: "If you’re unsure exactly how to take a medication, even if it was already explained to you, ask for clarification." That’s not just advice. It’s a survival tactic.
You’re not bothering anyone. You’re protecting yourself. The system is built for speed, not clarity. You have to be the one who slows it down to make sure it’s safe.
Next time you get a prescription, don’t just take it. Ask these three questions:
- What is this medicine for?
- Exactly how and when should I take it?
- What should I do if I miss a dose or feel side effects?
Write down the answers. Keep them with your pills. And if the answer still doesn’t make sense? Ask again. Until it does.



Jeremy Hernandez on 17 November 2025, AT 02:53 AM
They want us to ask questions? LOL. The system doesn’t want you to ask - it wants you to shut up and swallow the pill. Pharmacies are assembly lines, not clinics. They hand you the bottle like it’s a fast-food combo and hope you don’t die. I’ve seen pharmacists roll their eyes when you ask what 'BID' means. They’d rather you just guess and blame yourself when you get sick.