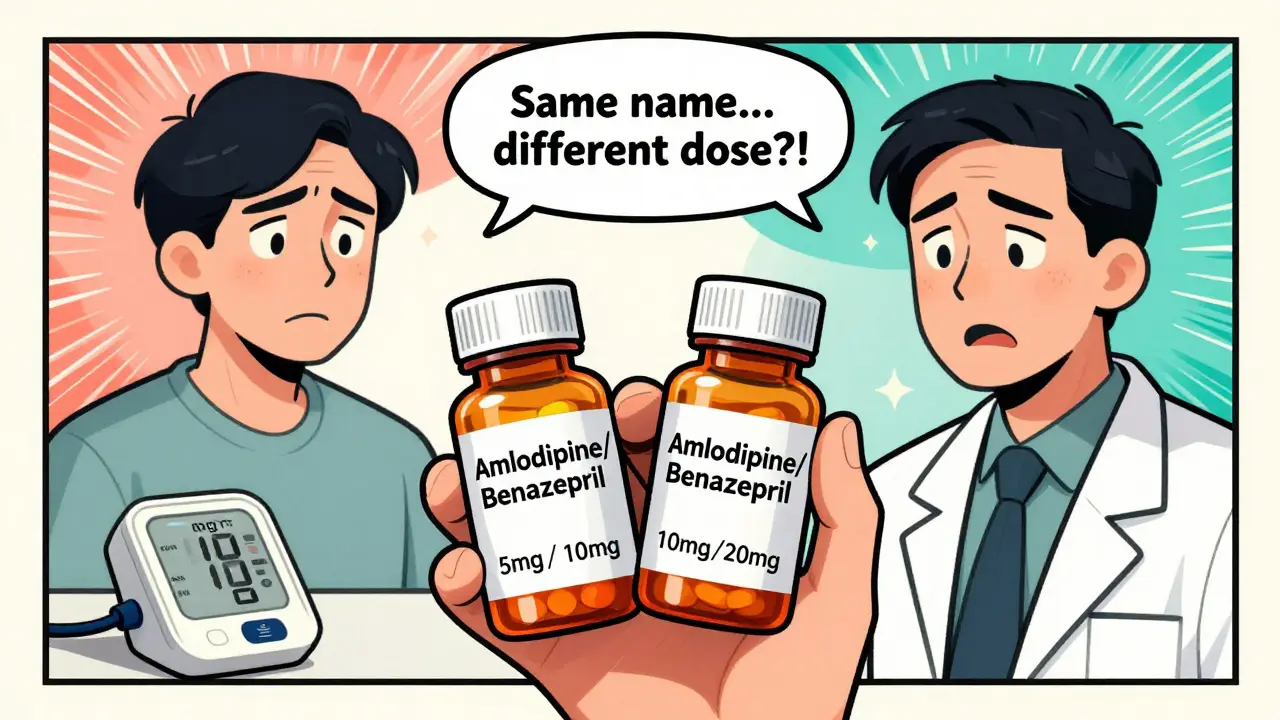
When a doctor writes a prescription for a drug like warfarin, lithium, or levothyroxine, they’re not just picking a medication-they’re managing a tightrope walk. These are Narrow Therapeutic Index (NTI) drugs, where even a small change in dose can mean the difference between effective treatment and dangerous toxicity. For patients on these medications, stability isn’t just preferred-it’s life-or-death. But when a pharmacist swaps the brand-name version for a cheaper generic, who’s really in control? And what do prescribers actually think about it?
The FDA defines NTI drugs as those where the gap between the minimum effective dose and the minimum toxic dose is extremely narrow-often less than a 2:1 ratio. That means if your blood level of phenytoin drops 10%, you might have a seizure. If it rises 10%, you could suffer neurological damage. This isn’t theoretical. Between 2015 and 2020, the Institute for Safe Medication Practices recorded over 1,200 medication errors linked to NTI drugs, with nearly 4 out of 10 tied to substitution. Eight percent led to real harm. That’s enough to make any clinician pause.
Doctors Don’t All Agree on Substitution
There’s no single prescriber voice on NTI substitution. Attitudes vary wildly by specialty, experience, and even geography. A 2018 survey of 710 pharmacists found that 94% believed physicians thought generic NTI drugs were just as safe as brand-name ones. But when you ask the doctors themselves, the picture changes. A 2023 American College of Physicians survey showed that 57% of internists would still choose the brand-name version when starting a high-risk patient on an NTI drug. Why? Stability. They’ve seen patients do well on one product-and they don’t want to risk rocking the boat.
Transplant specialists are even more cautious. Back in 1997, a survey of 59 transplant pharmacists found that 92% believed bioequivalence testing for drugs like tacrolimus should be done in actual patients, not healthy volunteers. Today, tacrolimus still holds a 32% brand-name market share despite generic availability. That’s not because generics don’t work-it’s because doctors who manage transplant patients have seen what happens when levels fluctuate. Rejection isn’t a minor side effect. It’s a crisis.
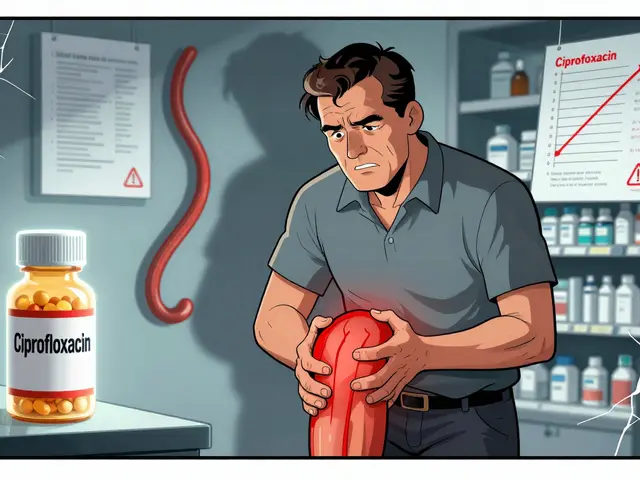
Neurologists feel the same way about levothyroxine and phenytoin. The American Academy of Neurology’s 2019 statement says automatic substitution for these drugs “may be inappropriate without prescriber consultation.” That’s not a recommendation-it’s a warning. One study found that 68% of physicians worried about INR fluctuations when switching warfarin generics. That’s not paranoia. It’s experience. INR levels are measured in decimals. A shift from 2.3 to 2.8 can mean the difference between preventing a clot and causing a bleed.
Pharmacists Are Doing Their Job-But It’s Not Always Welcome
Pharmacists aren’t the problem. They’re following the law and trying to save money. In fact, 82% of pharmacists almost always substitute generics for new NTI prescriptions. But here’s the twist: only 60% do it for refills. Why? Because they know the doctor might not want it. They’ve seen the calls. The confused patients. The extra lab tests.
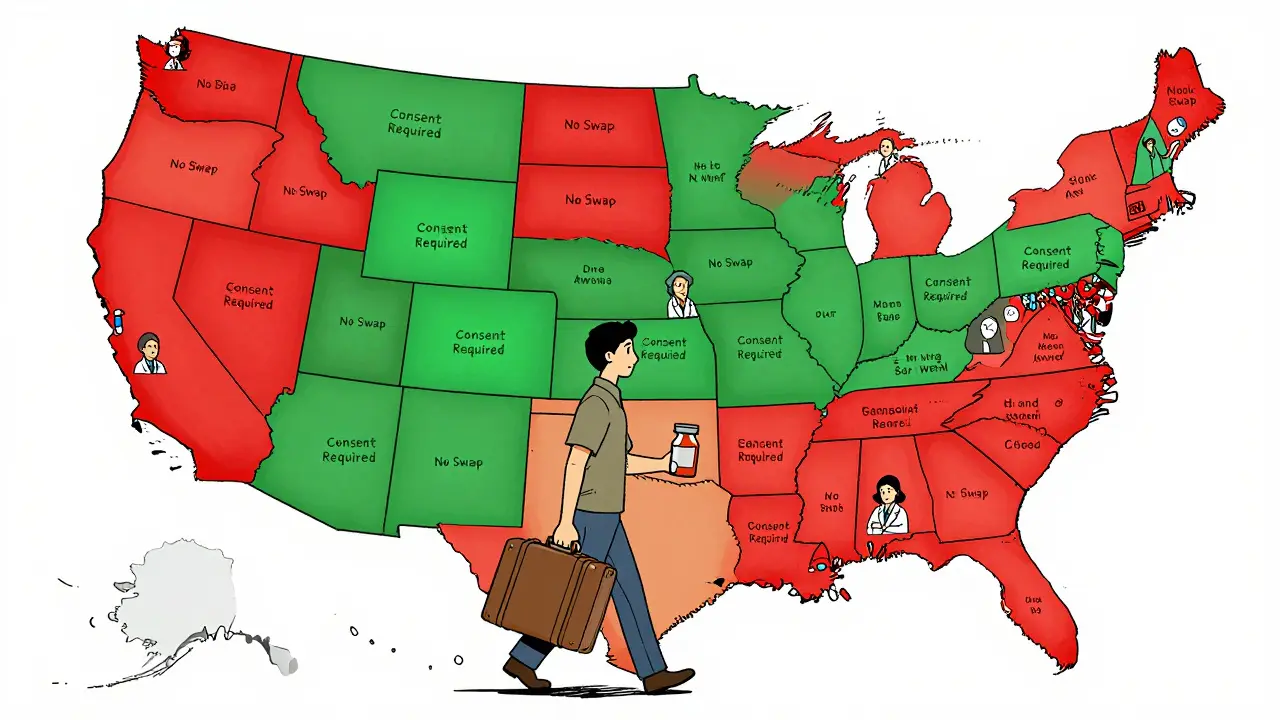
Hospital pharmacists report that 78% of them always notify the prescriber before swapping an NTI drug. That’s not standard practice for most medications. But for NTI drugs? It’s routine. In states like Texas and Florida, pharmacists can’t even substitute without prescriber approval. Seventeen states require explicit patient consent before switching. And guess what? Those states saw 23% fewer NTI substitutions than states without those rules.
But here’s where it gets messy: the FDA says 98% of generic NTI drugs perform within 3-4% of their brand-name counterparts. That’s solid. Post-market surveillance backs it up. So why the resistance? Because real patients aren’t lab rats. A patient on stable warfarin for five years isn’t the same as a healthy volunteer in a bioequivalence study. Their metabolism, diet, other meds, liver function-all of it matters. And when a generic switch causes a spike in INR, the doctor gets the call. Not the pharmacist. Not the insurance company. The doctor.
Communication Breakdowns Are Costing Time and Money
Prescribers aren’t resisting generics because they’re anti-savings. They’re resisting them because the system doesn’t support safe transitions. A 2021 study found that 63% of physicians prefer electronic notifications about NTI substitutions-not phone calls. But many pharmacies still rely on paper slips or outdated systems. Primary care doctors get an average of 2.7 NTI substitution alerts per month. Psychiatrists managing lithium? Five and a half. That’s not workflow. That’s noise.
And it’s expensive. The American Medical Association reports that 41% of physicians have seen patients confused after an NTI switch. Patients show up with questions, anxiety, or worse-symptoms from an unstable dose. Twenty-nine percent of prescribers say they’ve seen more office visits for monitoring after substitutions. Each one costs an estimated $127 in time, labs, and staff hours. Multiply that across thousands of patients, and you’re looking at millions in avoidable costs.
Dr. Michael Cohen of the Institute for Safe Medication Practices put it bluntly: prescribers need clearer labeling and standardized communication. Right now, there’s no consistent way to flag an NTI drug on a prescription. No universal code. No digital alert. It’s up to the pharmacist to know-and the doctor to remember. That’s not a system. That’s a gamble.
Regulation Is a Patchwork-And It’s Confusing
There are 28 U.S. states with specific NTI substitution rules as of 2023. Some require prescriber authorization. Others require patient consent. A few ban substitution entirely for certain drugs. The Academy of Managed Care Pharmacy opposes these restrictions, arguing pharmacists should use professional judgment. The American Society of Health-System Pharmacists says prescriber notification is essential. Meanwhile, the FDA maintains that generics are safe, and their 2023 update added 12 new drugs to the NTI list while removing three based on new data.
This isn’t just confusing for doctors. It’s chaotic for patients. Someone on tacrolimus in Florida might need a new prescription to switch generics. In California, they can swap without a word. And if they move? Their medication stability could be disrupted overnight. That’s not patient-centered care. That’s administrative roulette.
Why Do Brand-Name NTI Drugs Still Hold 23% of the Market?
Despite generics being cheaper and FDA-approved, brand-name NTI drugs still hold 23% of the market-nearly three times the rate of non-NTI drugs. Why? Because doctors are voting with their prescriptions. Tacrolimus, warfarin, levothyroxine, phenytoin, lithium-these are the top five. And in each case, a significant chunk of prescriptions still go to the brand.
It’s not about cost. It’s about control. When a patient is stable, doctors don’t want to risk a change. They don’t want to explain why their INR jumped. They don’t want to answer questions from anxious patients who read online that generics “aren’t the same.” And they don’t want to be the one held responsible if something goes wrong.
The Congressional Budget Office estimates that restricting NTI substitution could cost Medicare $1.2 billion a year. The generic drug industry says switching more could save $127 billion over ten years. But those numbers miss the human cost. The extra clinic visits. The anxiety. The near-misses. The errors that didn’t result in harm-but could have.
The Future: Better Data, Better Communication
Change is coming. The PRESCRIPT-NTI trial, enrolling 1,200 patients across 42 sites, is tracking real-world outcomes after substitution. Preliminary results are due in mid-2024. If the data shows no increased risk, attitudes may shift. The American Society of Clinical Oncology already supports generic substitution for oral cancer drugs-with monitoring. That’s progress.
Medicare’s November 2023 proposed rule now requires prescriber notification for all NTI substitutions under Part D. That’s a big step. It’s not a ban. It’s a checkpoint. A way to make sure the doctor knows what’s happening.
Industry analysts predict generic use for NTI drugs will rise to 78% by 2028. That’s up from 62% today. But that growth won’t come from forcing change. It’ll come from trust. Trust built on clear labeling, digital alerts, standardized protocols, and real-world evidence.
For now, the best path forward isn’t more rules. It’s better communication. It’s pharmacists and doctors talking-not just exchanging scripts, but sharing context. It’s patients being informed, not just notified. And it’s technology that doesn’t just track prescriptions, but understands them.
NTI drugs aren’t like other medications. They demand more than compliance. They demand coordination. And until the system catches up, prescribers will keep choosing the brand-not because they’re old-fashioned, but because they’ve seen what happens when the system fails.


vishnu priyanka on 14 January 2026, AT 06:18 AM
Man, I’ve seen this in India too - doctors here still prescribe brand-name warfarin even when generics are 80% cheaper. Patients don’t get it. They think ‘generic = fake.’ But honestly? If your INR’s stable and you’ve been on the same pill for years, why shake it up? It’s not about money, it’s about not turning a calm life into a medical rollercoaster.