Fluoroquinolone Tendon Risk Calculator
Risk Assessment Tool
Fluoroquinolones Can Cause Tendon Rupture-Even After You Stop Taking Them
You take an antibiotic because you’re sick. You expect to feel better. But what if the very drug meant to heal you could tear a tendon in your body? That’s not a hypothetical. It’s real. And it’s happening more often than most people realize.
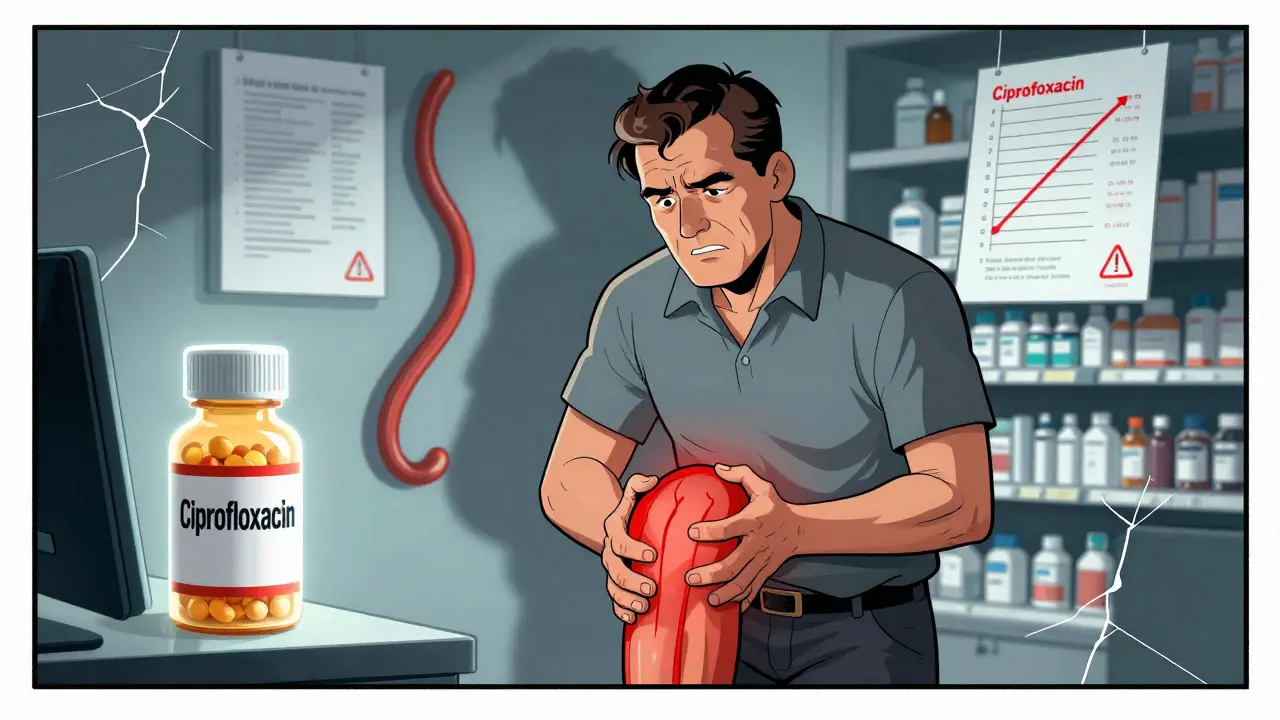
Fluoroquinolones-antibiotics like ciprofloxacin, levofloxacin, and moxifloxacin-are powerful. They’re used for serious infections: pneumonia, complicated urinary tract infections, even anthrax. But since the 2000s, evidence has piled up showing they carry a hidden, dangerous side effect: tendon damage. Not just pain. Not just inflammation. Actual rupture.
The Achilles tendon-the thick band connecting your calf to your heel-is the most vulnerable. Studies show it’s involved in nearly 90% of reported cases. And it doesn’t always happen while you’re still taking the drug. Symptoms can show up days after your last pill. Some people rupture their tendon weeks after finishing treatment. That’s why so many don’t connect the dots.
Who’s Most at Risk?
Not everyone who takes fluoroquinolones will have problems. But certain people are far more likely to. Age is the biggest factor. If you’re over 60, your risk jumps. Over 80? Your chance of rupture is more than 20 times higher than someone under 40.
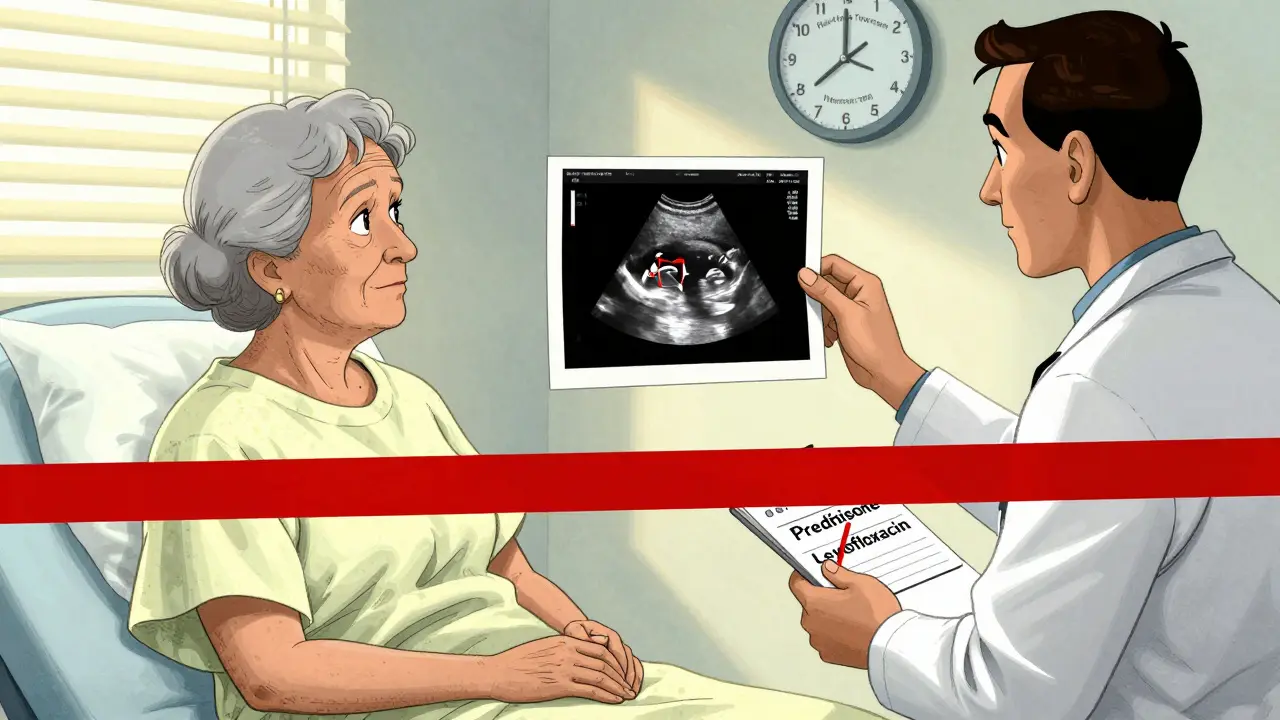
Then there’s corticosteroids. If you’re taking pills like prednisone for arthritis, asthma, or autoimmune conditions-and you’re prescribed a fluoroquinolone-your risk of tendon rupture goes up by 46 times. That’s not a typo. It’s not a small increase. It’s catastrophic.
Other high-risk groups include people with kidney disease, diabetes, or a history of tendon injury. Organ transplant recipients are also at higher risk, likely because they’re often on steroids and antibiotics together.
And yes, women appear to report these side effects slightly more often than men, though doctors still aren’t sure why. It’s not about dosage. It’s not about duration. Something deeper is at play.
How Fast Can It Happen?
Most people assume side effects show up after weeks. Not here. The median time from starting a fluoroquinolone to the first sign of tendon pain is just 6 days. Eighty-five percent of cases occur within the first month.
But the scariest part? One case documented tendon pain starting just two hours after taking the first pill. Another patient ruptured their Achilles tendon within a week of starting treatment. And if you ignore early warning signs-aching, swelling, stiffness-you could be one stumble away from a complete rupture.
And here’s the catch: tendon damage can happen even after you’ve stopped taking the antibiotic. The drug lingers in your system. The damage builds silently. That’s why doctors now warn patients to watch for symptoms for months after treatment ends.
Why Does This Happen?
Fluoroquinolones don’t just kill bacteria. They mess with your body’s own cells. They interfere with an enzyme called topoisomerase II, which your muscle and tendon cells need to repair DNA. When that enzyme is blocked, mitochondria-the energy factories in your cells-start to fail. Your tendons lose their ability to heal.
They also trigger inflammation at the cellular level, releasing toxic substances like nitric oxide and free radicals. These eat away at collagen, the protein that gives tendons their strength. And they bind to magnesium and calcium, which are critical for muscle-tendon signaling. Without those minerals, your tendons can’t respond properly to stress.
It’s not just one mechanism. It’s a cascade. And once it starts, it’s hard to stop.
The Numbers Don’t Lie
In the UK, a study of 6.4 million people found that those taking fluoroquinolones were more than four times as likely to develop tendinitis and twice as likely to suffer a full tendon rupture compared to those who didn’t take them.
A nationwide study in Taiwan followed over 350,000 people. Those on fluoroquinolones had a 42% higher rate of tendon disorders than those who weren’t. And half of all ruptures happened within the first week of starting the drug.
Even more telling? The FDA’s own database shows tendon pain and tendinitis are among the top five most-reported side effects of fluoroquinolones-right behind joint pain and limb discomfort. These aren’t rare. They’re common enough to force global regulatory action.
What Do Health Agencies Say Now?
Back in 2008, the U.S. Food and Drug Administration slapped a black-box warning on fluoroquinolones-the strongest warning they can give. It said: “Tendon rupture can occur in patients of any age, but risk increases with age over 60, corticosteroid use, and kidney disease.”
In 2013, they strengthened it. In 2018, they updated patient guides and sent them to over 6,000 clinics. The message: Don’t take this unless you absolutely have to.
The UK’s MHRA did the same in 2019. They now say fluoroquinolones should only be used for serious infections when no other antibiotic will work. Same in Europe. The European Medicines Agency restricted them too.
And the Infectious Diseases Society of America now recommends fluoroquinolones be a third-line option-only after first- and second-line antibiotics have failed.
What Should You Do If You’re Prescribed One?
Don’t panic. But don’t ignore the warning signs either.
- Ask your doctor: “Is there another antibiotic I can take?”
- Check your meds: Are you on steroids? Do you have kidney issues or diabetes? If yes, push back.
- Know the symptoms: Pain, swelling, or stiffness in your Achilles, shoulder, or hand tendons. It might feel like a dull ache at first. Then it gets worse with movement.
- Stop the drug immediately if you feel tendon pain. Don’t wait. Don’t tough it out. Call your doctor. Get an ultrasound or MRI. Early intervention can prevent a full rupture.
- Avoid exercise. If you’re on a fluoroquinolone, skip running, jumping, heavy lifting. Even walking too much can strain a weakened tendon.
And if you’re already done with the course? Keep watching. Tendon rupture can happen weeks later. If you feel sudden, sharp pain in your heel or shoulder-especially if it’s accompanied by a popping sound-get to a doctor right away.
There’s a Better Way
Fluoroquinolones are powerful. But they’re not always necessary. For most urinary tract infections, simple antibiotics like nitrofurantoin or trimethoprim work just as well-with far fewer risks. For sinus infections, amoxicillin or doxycycline are safer bets.
Doctors still prescribe fluoroquinolones too often. Too easily. Too quickly. Partly because they’re broad-spectrum. Partly because they’re convenient. But the cost-permanent disability-is too high.
Patients need to be partners in this decision. If your doctor reaches for ciprofloxacin for a mild infection, ask: “Is this really the best choice?”
What If You’ve Already Had a Tendon Injury?
If you’ve had a tendon rupture linked to fluoroquinolones, you’re not alone. Many people recover with physical therapy and rest. But some never fully regain strength. Some need surgery. A few end up with chronic pain for life.
There’s no cure for fluoroquinolone-induced tendon damage. Only management. And prevention is the only real defense.
Document your experience. Tell your doctor. Report it to your country’s drug safety agency. The more data we collect, the harder it becomes for the medical system to ignore.
Final Thought: Your Tendons Are Not Disposable
Antibiotics save lives. But they’re not harmless. Fluoroquinolones are a reminder that powerful drugs come with powerful risks. Your tendons carry your body. They let you walk, run, climb, lift. They’re not meant to be collateral damage.
If you’re prescribed a fluoroquinolone, don’t just sign the prescription. Ask questions. Push for alternatives. Listen to your body. And if you feel pain in your tendons-no matter how small-take it seriously. It could be the warning before the rupture.
Can fluoroquinolones cause tendon rupture even after stopping the drug?
Yes. While most tendon problems start during treatment, symptoms-including rupture-can occur weeks or even months after stopping the antibiotic. The drug can linger in tissues and continue to disrupt tendon repair for a long time. This delayed onset is why doctors now warn patients to monitor for pain for up to six months after finishing the course.
Which fluoroquinolone has the highest risk of tendon damage?
Levofloxacin is linked to the most cases of tendon injury, followed by ciprofloxacin. Moxifloxacin carries a lower but still significant risk. All fluoroquinolones in this class carry the same black-box warning, but real-world data shows levofloxacin and ciprofloxacin are involved in over 88% of reported tendon ruptures.
Are there safer antibiotics for treating UTIs or sinus infections?
Yes. For most uncomplicated urinary tract infections, nitrofurantoin or trimethoprim are first-line and carry no tendon risk. For sinus infections, amoxicillin or doxycycline are preferred. Fluoroquinolones should only be used if these fail or if the infection is severe, complicated, or resistant to other drugs.
Why does the Achilles tendon get hurt more than other tendons?
The Achilles tendon has relatively poor blood supply compared to other tendons, making it slower to repair. It also bears the most mechanical stress during daily movement. When fluoroquinolones weaken tendon structure and impair healing, the Achilles is the first to fail under normal use. Studies show it’s involved in nearly 90% of cases.
Should I avoid fluoroquinolones if I’m over 60?
Yes, unless it’s a life-threatening infection. The risk of tendon rupture increases dramatically after age 60, especially if you’re also on steroids or have kidney disease. Doctors should always explore safer alternatives first. If no other option exists, the lowest effective dose for the shortest possible time should be used-with close monitoring.
What should I do if I feel tendon pain while taking a fluoroquinolone?
Stop taking the antibiotic immediately and contact your doctor. Do not wait to see if it gets better. Tendon pain is a warning sign-not a side effect to tolerate. Get imaging (ultrasound or MRI) to check for inflammation or early tearing. Rest the affected area. Avoid weight-bearing or strenuous activity. Early action can prevent a full rupture.
Is there a way to reverse fluoroquinolone tendon damage?
There’s no proven treatment to reverse the damage. Once collagen structure is degraded, it doesn’t fully regenerate. Recovery relies on rest, physical therapy, and sometimes surgery. Some patients regain function, but many live with chronic pain or weakness. Prevention is the only reliable strategy.
Can I take fluoroquinolones if I’ve had a tendon rupture before?
No. If you’ve had a fluoroquinolone-related tendon rupture in the past, you should never take this class of antibiotics again. The risk of re-rupture is extremely high. Inform all future providers of your history. Alternative antibiotics are always preferred.

clarissa sulio on 2 February 2026, AT 01:23 AM
This is why we need to stop letting pharmaceutical companies dictate our healthcare. They push these drugs like candy and then act shocked when people end up in wheelchairs. We need stricter regulations, not just warnings.