Out of all the pills you’ll ever come across, few have made as big a splash as chloroquine. Imagine one drug that’s been a hero against malaria, a hot debate during a worldwide pandemic, and now, in 2025, still manages to get people talking. How did a medication invented before color television become part of our routines and controversies? Whether you’ve heard whispers about it curing everything, or you’re plain worried about side effects, this is the no-nonsense breakdown that finally sorts fact from fiction.
Chloroquine: The Pill That’s Been Everywhere
If you grew up in an area where mosquitoes rule, chloroquine is almost as famous as aspirin. Developed in the 1930s and rolled out after World War II, this drug turned malaria from a guaranteed misery into something doctors could manage. Malaria, thanks to those relentless little Anopheles mosquitoes, has long been the bane of tropical and subtropical regions.
Chloroquine works by ruining the digestion party inside the malaria parasite’s stomach. When the parasite invades your red blood cells and tries converting hemoglobin into protein, chloroquine crashes the process. It’s almost poetic: a parasite kills itself by trying to eat you.
For decades, anyone traveling to, working in, or living near the equator probably took chloroquine. It was cheap, easy to make, and compared to earlier concoctions—think arsenic-based treatments—it actually kept people alive. By the 1970s, widespread chloroquine use had saved millions.
But things started to get bumpy. Mosquitoes kept biting, and the malaria parasite wasn’t slouching. By the late 20th century, resistance set in. Regions like Sub-Saharan Africa saw massive drops in chloroquine effectiveness. By 2000, doctors in these places switched to alternatives like artemisinin-based combos.
If you’re planning a trip to the Amazon, Southeast Asia, or Africa today, your doctor probably won’t hand you chloroquine. Yet, in certain spots—a few places in Central America, parts of the Caribbean, and some zones in the Middle East—the parasite hasn’t outsmarted it yet. Bottom line? Always check the up-to-date resistance maps before popping any antimalarial.
Now, just when you thought medical history couldn’t twist any further, along comes COVID-19. Remember the wild days of 2020? Chloroquine (and cousin drug hydroxychloroquine) was everywhere in the news. Social media called it a miracle cure. The president of the United States touted it during press conferences. Pharmacies sold out. What most people missed: early laboratory results looked promising, but real-world trials kept coming up short. Major studies published in ‘The New England Journal of Medicine’ by spring 2020 showed no meaningful benefit for COVID-19 patients. As of today in 2025, official health authorities worldwide do not recommend chloroquine for COVID-19 prevention or treatment.
But the drug’s usefulness isn’t dead. Autoimmune patients, like those with lupus or rheumatoid arthritis, still rely on hydroxychloroquine (a close sibling) to tamp down their immune systems and ease joint pain. The journey from malaria pill to pandemic headline has made chloroquine one of the most recognizable prescriptions outside a pharmacy textbook.

How Chloroquine Fits Into Your Life: Uses, Dosage, and Tips
So, who actually needs chloroquine today? Its main claim to fame is malaria prevention and treatment. If you’re in a country or region where malaria is still a threat and chloroquine resistance is low, doctors might suggest taking it weekly as a preventive. For actual malaria cases sensitive to chloroquine, a short course knocks out the infection. Don’t get creative with the dosage—more isn’t better, since this drug has a narrow safety margin.
Doctors also rely on a close cousin, hydroxychloroquine, for people with autoimmune diseases, like lupus and rheumatoid arthritis. It tamps down an overactive immune system. You’ll find hydroxychloroquine prescribed much more often these days, especially for long-term, low-dose therapy because it’s a bit gentler on the body.
If you’re prescribed chloroquine, timing matters. Preventive dosing starts one week before traveling to a malaria zone and continues for four weeks after you leave. Forgetting pills is a classic fail. Folks in the U.S. who picked up malaria almost always skipped or mis-timed their doses. Set a weekly reminder—your body will thank you.
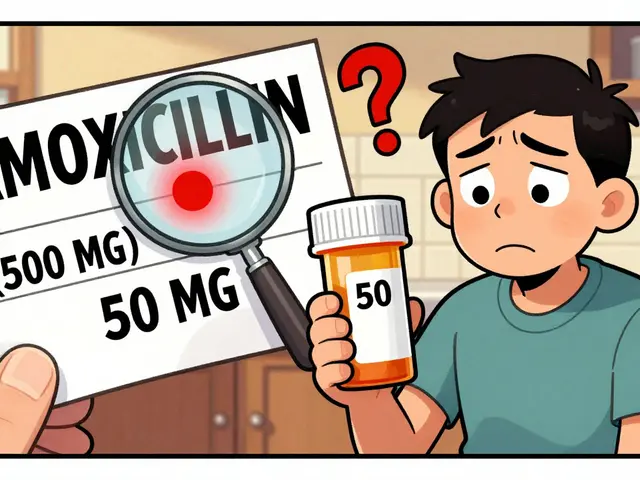
Side effects? You want the real deal. Common reactions can range from minor tummy upset, skin rashes, and headaches to more worrying stuff like vision changes, mood swings, or heart rhythm problems. Eye issues get their own spotlight: long-term use can cause damage to the retina, so regular eye exams matter for anyone on this drug for longer stretches. Rare but dangerous effects include seizures, severe allergic reactions, and, with big overdoses, even death. That’s why you never want to double up a missed dose.
People with certain conditions need extra caution. Got a personal or family history of heart issues, especially irregular heartbeats (QT prolongation)? Make sure your doctor knows. Those with psoriasis, liver or kidney problems, or blood disorders should have a full discussion before starting chloroquine. And if you’re on any other meds—heart drugs, antibiotics like azithromycin, or even allergy relief—let your doctor know about every single pill. Drug interactions can get dicey.
Pregnant but worried about malaria? Chloroquine actually rates as one of the safest malaria drugs during pregnancy. Decades of use back up its safety record. But breastfeeding or postpartum—again, it often passes through in very small amounts, and most guidelines still allow for use if you need it to prevent or treat malaria.
Never buy chloroquine over-the-counter from sketchy websites. Counterfeits have popped up everywhere from Nigerian markets to online pharmacies that barely exist. Real chloroquine pills have an unmistakable bitter taste, but the only way to be sure is via regulated, trusted suppliers.
As for special instructions, take with food to prevent stomach upset, and always wash down with a full glass of water. Don’t crush or chew the tablets. If you miss a dose, take it as soon as you remember but skip it if it’s almost time for the next. And never, ever, double up.
Travel advice: If you’re headed somewhere with malaria, double-check your travel medicine plan. New malaria-resistant strains sometimes emerge fast. Each year, organizations like the CDC and WHO update malaria maps and drug guidelines—don’t rely on last year’s advice.
| Year | New Malaria Cases (in millions) | Chloroquine Resistance |
|---|---|---|
| 1960 | 100 | Rare |
| 1980 | 200 | Central Africa & Southeast Asia |
| 2000 | 230 | Widespread in Africa |
| 2024 | 249 | Persistent in Africa, lower in Central America |
Myths, Media Storms, and the Truth in 2025
Chloroquine has had a wild ride—one minute it’s a basic medicine in rural clinics, the next it’s headline news and a lightning rod for rumors. So what’s true, what’s hype, and what should you do in 2025 if you hear fresh chatter about this famous pill?
One stubborn myth: Chloroquine can treat every strain of malaria. Not true. Some strains, especially in Africa and Asia, have outsmarted it. Others, mostly in a few islands and parts of Central America, are still vulnerable. Taking chloroquine in a resistant zone won’t protect you, and it can make you act like you’re invincible—only to get smacked with malaria anyway.
Another big misconception was that it was a miracle fix for COVID-19, like a genie in a bottle for a scary virus. But as more rigorous studies came in, ranging from the WHO Solidarity Trial to that major NEJM report in spring 2020, nearly all showed it didn’t change outcomes for COVID-19 patients. And side effects—especially when mixed with other drugs—became a real risk.
Something people often forget: Even well-known drugs can be dangerous. Chloroquine is safer than some of its historic malaria medicine siblings, sure, but overdose is no joke. Just 20 grams (roughly a handful of tablets) can be deadly to adults. There’s even a dark history in the 1970s and 80s of intentional overdoses in Europe and Australia. Hospitals have protocols now, but the danger is still very real. That’s why, now in 2025, many countries strictly control access and don’t let you grab it without a prescription.
Misinformation online isn’t just annoying—it’s actually dangerous. From fake COVID treatments to “immunity booster” scams, chloroquine headlines have fueled all kinds of shady business. The trick? Fact-check. Stick to reliable medical sources: think CDC, WHO, or your country’s health ministry. And never swallow some powder mailed from a faceless seller in another country.
Here’s a practical tip if you’re prescribed chloroquine: always keep it out of reach from kids. The tablets can look like regular medicine or even candy to small children, and accidental ingestion can be fatal. If a child swallows even a single adult dose, get emergency help instantly.
If you're the type who loves reading labels or asking your doctor lots of questions, you’re already ahead. Bring up any history of eye issues, seizures, or allergies. If you wear contacts or have had an eye exam in the last year, mention it—retinal side effects depend a lot on your health background. Also, don’t skip the bloodwork and ECGs if your doctor orders them. Early detection makes side effects way easier to handle.
Curious about travel safety? If you’re going somewhere exotic, get updated travel guidance from your clinic or a travel health website about a month before your departure. And bring your own meds, since counterfeit malaria drugs remain a problem in many countries and border shops.
Pro tip for long-term chloroquine users: schedule regular eye checks every 6-12 months. Subtle vision changes or color vision shifts can mean rare but serious side effects. Early caught, they’re often reversible, but if ignored, you can get lasting damage. Don’t self-adjust your dose if you feel fine—side effects can sneak up slowly, with no warning signs until the damage is there.
And about mixing medications—chloroquine doesn’t always play nice. Tell your provider about every supplement, prescription, herbal remedy, or street drug you use; even seemingly innocent stuff can throw off your heart rhythm or affect chloroquine levels.
For folks in parts of the world where malaria is still everywhere in 2025, the bigger question might be access. Given resistance, price spikes, and shipping issues, sometimes the real challenge is just staying supplied. If you’re worried about cost or counterfeit meds, check if your country offers subsidized or free medication programs, or ask your pharmacist where to find regulated pills. It’s far safer than risking random supplies or crossing borders with uncertain packages.
You don’t need to be a pharmacist to stay safe: take it as prescribed, ask questions, keep up with new malaria resistance reports, and steer clear of miracle-cure hype online. Chloroquine’s story isn’t about to end anytime soon, and in the right hands, it’s still a lifesaver.



Richard Phelan on 13 August 2025, AT 18:36 PM
Nice write-up — solid overview and no nonsense, I like that.
A couple of quick grammar nags: "rolled out after World War II" reads fine, but the sentence flow in the paragraph about resistance jumps a little — maybe tighten the transition there. Also, that table is handy but the header cells could use clearer units (millions is only on one column).
Content-wise: totally agree with the emphasis on resistance maps and not buying pills from random online vendors. That advice alone could save people from catastrophe.