When antibiotics disappear from hospital shelves, it’s not just a supply chain hiccup-it’s a life-or-death emergency. In 2023, antibiotic shortages affected one in six bacterial infections globally, according to the World Health Organization. For urinary tract infections, that number jumped to one in three. These aren’t hypothetical risks. They’re happening right now-in clinics, emergency rooms, and rural health centers from Bristol to Bangladesh.
Why Antibiotics Are More Likely to Vanish Than Other Drugs
Antibiotics are 42% more likely to face shortages than any other type of medication. Why? It’s not because they’re harder to make. It’s because no one wants to pay for them. Generic antibiotics, which make up 85% of global use, have seen their prices drop by 27% since 2015. Meanwhile, the cost to meet strict manufacturing standards for sterile injectables has gone up 34%. Manufacturers are caught in a trap: they can’t make money selling cheap antibiotics, but they can’t afford to stop making them either.The result? Production lines shut down. A single factory in India or China that stops producing penicillin G benzathine-a drug used to treat strep throat and prevent rheumatic heart disease-can trigger shortages across continents. The U.S. had 147 active antibiotic shortages by the end of 2024. In the UK, shortages more than doubled after Brexit, rising from 648 in 2020 to 1,634 in 2023. The European Economic Area reported 28 countries in crisis, with 14 calling their shortages “critical.”
What Happens When Amoxicillin or Penicillin Isn’t Available
Imagine your child has pneumonia. The doctor prescribes azithromycin. But the pharmacy has none. No stock. No backorder. No alternative that works as well. That’s not fiction. In Mumbai, a mother waited 72 hours for her child’s antibiotic. By then, the infection had worsened. The child ended up in intensive care.When amoxicillin runs out, doctors don’t just switch to another pill. They often turn to broader-spectrum antibiotics like carbapenems-drugs meant for last-resort cases. But using them too early speeds up resistance. In 2023, over 40% of E. coli and 55% of K. pneumoniae were already resistant to third-generation cephalosporins. When those fail, carbapenems become the only option. And when carbapenems run out? Clinicians are left with colistin-a toxic, decades-old drug that can damage kidneys and nerves.
A doctor in California told the American Public Health Association she had to give colistin for a routine urinary tract infection. A UK physician on Reddit wrote about rationing amoxicillin. In rural Kenya, nurses send patients home without treatment because penicillin isn’t there. These aren’t rare cases. A 2025 survey found 78% of U.S. hospital pharmacists changed treatment plans because of shortages. Sixty-two percent saw more patients get sicker as a result.
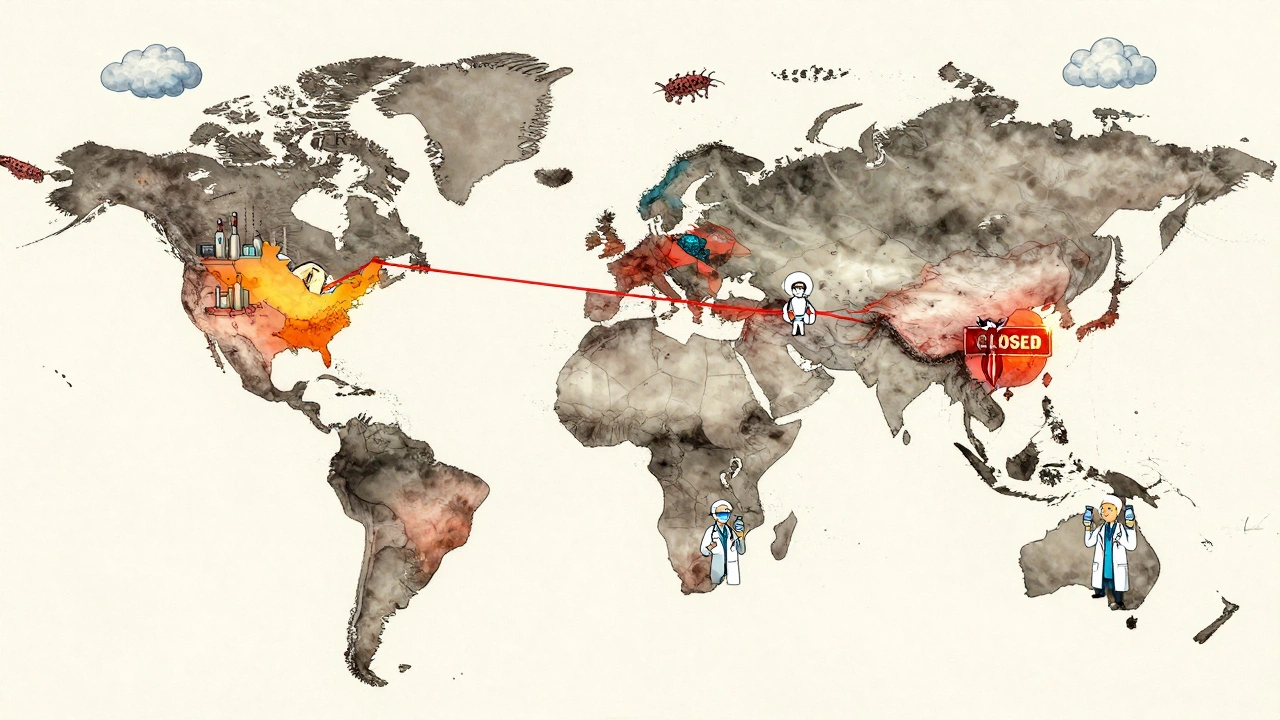
The Global Inequality of Antibiotic Access
High-income countries can sometimes import antibiotics or scramble to find substitutes. But in low- and middle-income countries, the problem is worse. Seven out of ten people in these regions already can’t get the antibiotics they need. Now, with global supply chains strained, that number is climbing.The WHO calls this a “syndemic”-a deadly mix of antibiotic resistance and under-treatment. In places with weak health systems, a simple infection like a skin abscess or a urinary tract infection can turn fatal. There’s no backup plan. No insurance. No pharmacy down the street. No emergency stockpile. And no one is tracking how many people die because of it.
Meanwhile, in wealthier nations, the crisis is hidden in plain sight. Hospitals are forced to ration. Pharmacists spend extra hours tracking down drugs. Doctors delay treatments. Patients get sicker. The American Society of Health-System Pharmacists found that pharmacists now spend 22% more time just managing shortages. That’s time taken away from counseling patients, checking for interactions, or ensuring safe dosing.
What’s Being Done-and Why It’s Not Enough
The WHO launched a five-point action plan in October 2025, including a $500 million Global Antibiotic Supply Security Initiative by 2027. The U.S. FDA approved two new manufacturing facilities in early 2025, expected to ease 15% of shortages by the end of the year. The European Commission is pushing its Pharmaceutical Strategy for Europe to fix supply chains by 2026.But these are band-aids on a bleeding wound. The global antibiotic market grew just 1.2% from 2019 to 2024-far below the 5.7% average for all pharmaceuticals. Companies invest in cancer drugs, diabetes meds, and rare disease treatments because they’re profitable. Antibiotics? Not so much.
Even when hospitals try to respond, they struggle. Only 37% of U.S. hospitals meet all WHO standards for antimicrobial stewardship programs-programs that track how antibiotics are used and try to prevent waste and misuse. Johns Hopkins reduced unnecessary broad-spectrum antibiotic use by 37% during shortages by using rapid diagnostic tests. But most hospitals don’t have that tech. Or the staff. Or the funding.
Regional sharing networks, like the one started in California in 2024, have cut critical shortage impacts by 43%. But they’re rare. And fragile. What happens when three states run out at once?

The Real Cost: More Deaths, More Resistance
Every time an antibiotic isn’t available, two things happen: people suffer, and bacteria evolve. The Review on Antimicrobial Resistance predicts that without major intervention, antibiotic shortages will grow by 40% by 2030-and cause 1.2 million more deaths each year from infections we used to treat easily.And resistance isn’t slowing. Between 2018 and 2023, resistance rose in over 40% of the pathogen-antibiotic pairs the WHO monitored. The average annual increase? 5% to 15%. We’re running out of options faster than we’re making new ones. Only 58% of global antibiotic use currently comes from the WHO’s “Access” group-drugs that are effective, safe, and less likely to drive resistance. The target is 70% by 2030. We’re falling behind.
Meanwhile, the drugs we rely on most-amoxicillin, penicillin, ciprofloxacin-are aging. Their patents expired decades ago. No one is incentivized to improve them. No one is investing in new versions. The pipeline is dry.
What Can Be Done Now?
There’s no single fix. But there are steps that work:- Build regional stockpiles of critical antibiotics-especially for injectables like penicillin and ampicillin.
- Pay manufacturers fairly for producing essential antibiotics, even if they’re cheap. Governments can guarantee minimum purchase volumes.
- Expand rapid diagnostics so doctors don’t guess. If you know it’s a virus, don’t give an antibiotic. If you know it’s resistant, avoid the wrong drug.
- Protect the “Access” group of antibiotics. These are the ones we need most. Don’t let them be replaced by broad-spectrum drugs unless absolutely necessary.
- Support global surveillance. The WHO’s GLASS system now covers 104 countries. That’s progress. But we need real-time data, not annual reports.
Antibiotics are not like painkillers or blood pressure pills. They’re our last line of defense against bacterial infections. When they vanish, we don’t just lose a treatment-we lose the ability to safely perform surgeries, deliver babies, treat cancer, and care for premature infants. The next time you hear about a drug shortage, don’t think of it as a logistics problem. Think of it as a public health emergency. Because it is.



Lara Tobin on 13 December 2025, AT 00:46 AM
This hit me hard. I had a friend whose kid got sepsis last year because the local pharmacy ran out of amoxicillin. They drove 90 miles to find it. No one talks about this enough. 😔