Ringworm isn’t caused by a worm at all. Despite the name, it’s a common fungal infection that affects the skin, scalp, or nails. You might see a red, circular rash with a clear center and raised, scaly edges - that’s the classic sign. But ringworm can also look like dry, flaky patches, stubborn athlete’s foot between the toes, or thick, discolored nails. It’s contagious, frustrating, and often misunderstood. The good news? Most cases clear up quickly with the right treatment - if you catch it early and stick with it.
What Exactly Is Ringworm?
Ringworm, medically called dermatophytosis or tinea, is caused by a group of fungi called dermatophytes. These aren’t worms - they’re mold-like organisms that feed on keratin, a protein found in skin, hair, and nails. The three main culprits are Trichophyton, Microsporum, and Epidermophyton. They thrive in warm, damp places: locker rooms, public showers, gym mats, and even your own sweaty socks. The infection gets its name from the ring-shaped rash it often forms, but not all cases look like that. Sometimes it’s just a red, itchy patch that slowly spreads. The Centers for Disease Control and Prevention estimates that 20-25% of people worldwide will get ringworm at some point. In the U.S. alone, about 40 million cases are reported every year.Types of Tinea Infections - And Where They Show Up
Ringworm isn’t one single thing. It changes based on where it lands on your body:- Tinea corporis (body ringworm): Red, circular, itchy rash with a raised border. Starts small - about half an inch - and grows outward. Common on arms, legs, and torso.
- Tinea pedis (athlete’s foot): Affects feet, especially between the toes. Skin peels, cracks, or blisters. Often smells bad. Causes burning or stinging. Accounts for 15% of all ringworm cases.
- Tinea cruris (jock itch): Red, itchy rash on the inner thighs, groin, or buttocks. More common in men, especially those who sweat a lot or wear tight clothing.
- Tinea capitis (scalp ringworm): Mostly affects children. Causes scaly, red patches on the scalp, hair loss, and sometimes a swollen, pus-filled lump called a kerion. Can lead to permanent scarring if untreated.
- Tinea unguium (nail fungus): Nails become thick, yellow or brown, brittle, and crumbly. Toenails are three times more likely to be affected than fingernails because shoes create a perfect humid environment for fungi.
How Do You Get It?
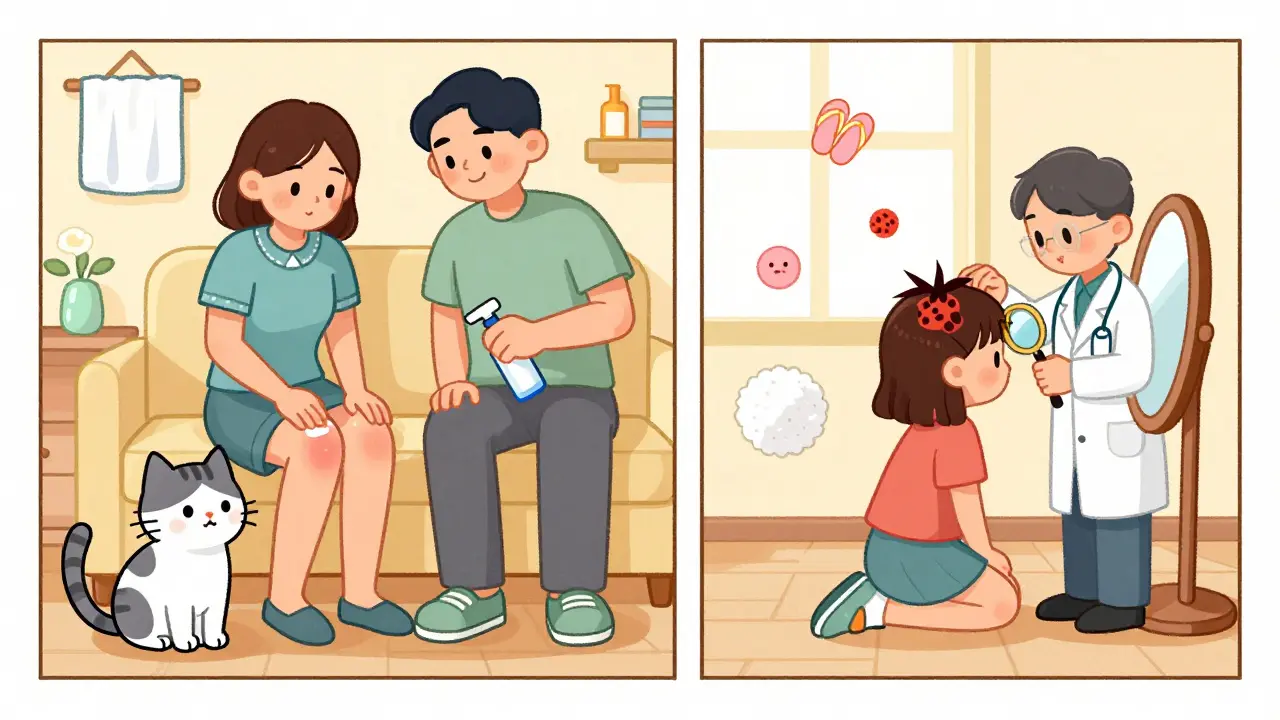
You don’t need to be dirty to get ringworm - you just need to be exposed. Transmission happens in three main ways:- Skin-to-skin contact (60% of cases): Touching someone with ringworm - or even a pet with a patchy coat.
- Contaminated surfaces (30%): Walking barefoot in a locker room, sharing towels, using a gym mat, or wearing someone else’s shoes.
- Animal contact (10%): Cats, dogs, and rodents can carry the fungus. Veterinarians and pet owners have a 15-20% higher risk.

Antifungal Creams - What Works and What Doesn’t
For most skin and nail infections, topical creams are the first step. They’re cheap, easy to use, and effective - if you use them right. Here are the top four active ingredients in over-the-counter antifungal creams:- Clotrimazole (1%): Works in 70-80% of cases. Apply twice daily for 2-4 weeks. Slower to show results - improvement may take 7-10 days.
- Miconazole (2%): Similar effectiveness to clotrimazole. Often found in combination with hydrocortisone to reduce itching.
- Terbinafine (1%): The fastest and most effective. Studies show 80-90% success rate. Many users see improvement in just 3-5 days. Brand name Lamisil AT. Average Amazon rating: 4.3/5 stars.
- Ketoconazole (2%): Effective at 75-85%. Often used for stubborn cases or when other creams fail.
One big mistake? Stopping treatment too soon. A 2023 Reddit thread with over 1,200 comments found that 68% of users stopped applying cream once the rash looked better. Result? 45% of them got it back. Fungi don’t vanish just because the redness fades. You need to kill every last spore.
For scalp infections (tinea capitis) or severe nail fungus, creams won’t cut it. Oral medications like terbinafine (250mg daily) are required. These work from the inside out and cure 85-90% of scalp cases. But they come with side effects - liver enzyme changes, nausea, headaches - so they’re only prescribed when necessary.
What About Natural Remedies?
Tea tree oil, coconut oil, apple cider vinegar - you’ve probably heard they help. But here’s the truth: a 2021 Cochrane Review found no strong evidence that natural remedies are as effective as pharmaceutical antifungals. Tea tree oil (5-10%) cleared the infection in only 40-50% of cases, compared to 70-90% for clotrimazole or terbinafine. Some people swear by them. But if you’re dealing with a spreading rash, a bald patch on your child’s head, or thickened nails, don’t gamble. Delaying proper treatment can lead to permanent damage - especially with scalp ringworm.Prevention - Stop It Before It Starts
Preventing ringworm is easier than treating it:- Wear flip-flops in public showers, pools, and gyms. Reduces risk by 45%.
- Change socks daily - twice a day if you sweat a lot.
- Avoid sharing towels, combs, hats, or shoes.
- Keep skin dry. Use talcum powder in sweaty areas like feet and groin.
- Wash athletic gear after every use. Fungi live in damp fabric.
- Check pets for bald spots or flaky skin. If your cat has a patchy coat, take it to the vet.
Parents of school-age kids should know: 15-20% of elementary schools have at least one ringworm outbreak every year. It spreads fast in locker rooms and shared equipment. Teach kids not to share hairbrushes or helmets.
When to See a Doctor
Most ringworm cases can be handled at home. But call your doctor if:- The rash doesn’t improve after 2 weeks of antifungal cream.
- It spreads rapidly or gets worse - especially if it becomes painful, swollen, or oozes.
- You have a bald patch on your child’s scalp. That’s tinea capitis - needs oral meds.
- Your nails are thick, discolored, and painful. Nail fungus is hard to treat without prescription drugs.
- You’re immunocompromised. People with diabetes, HIV, or on steroids have a 3.5x higher chance of treatment failure.
Doctors can confirm the diagnosis with a skin scraping or fungal culture. It’s not always ringworm - psoriasis, eczema, and bacterial infections can look similar. Misdiagnosis leads to wrong treatment and longer suffering.
Cost, Time, and Real-World Results
Over-the-counter antifungal creams cost $5-$15 per tube (average $8.75). Prescription oral meds run $25-$150 depending on insurance. The total U.S. cost for treating ringworm is about $500 million a year. Most people see improvement within 3-7 days with terbinafine. Full clearance usually takes 2-3 weeks. But if you stop early, you’re likely to relapse. And relapses mean more money, more time, and more frustration.Why This Matters Beyond the Itch
Ringworm isn’t just a nuisance. For teenagers, visible rashes on the face or arms can lead to bullying. A 2022 Kids Health survey found 73% of affected adolescents reported being teased or isolated. For athletes, it can mean being benched. For parents, it means school absences and vet bills. The good news? Ringworm is one of the most treatable skin conditions out there. With the right cream, consistent use, and smart prevention, you can get rid of it - and keep it from coming back.Can ringworm go away on its own without treatment?
Sometimes, yes - but it’s risky. Left untreated, ringworm can spread to cover 30-50% more skin area in just two weeks. It can also infect others in your household or spread to your scalp or nails, which are much harder to treat. Plus, the longer it stays, the higher the chance of scarring, especially in children with scalp infections. Treatment cuts healing time by 5-7 days and prevents complications.
Is ringworm contagious to pets?
Yes. Cats, dogs, and rodents can carry and spread the fungus. You can get it from them, and they can get it from you. If you have ringworm and own a pet with patchy fur, flaky skin, or excessive scratching, take them to the vet. Treating both the person and the pet is often necessary to stop the cycle.
Why does my ringworm keep coming back?
Most often, it’s because you didn’t finish the treatment. Fungi can hide deep in skin layers even after the rash looks gone. Stopping cream too early leaves spores alive. Other reasons: re-exposure (e.g., walking barefoot in the same shower), sharing towels, or not washing bedding and clothes during treatment. To prevent recurrence, treat for the full 2-4 weeks and disinfect everything you touch.
Can I use antifungal cream on my face?
Some antifungal creams are safe for the face, but not all. Avoid products with corticosteroids (like hydrocortisone) on your face - they can thin the skin and worsen the infection. Use only creams labeled for facial use or ask your doctor. Facial ringworm can look like acne or eczema, so get it confirmed before treating.
Do I need to throw away my shoes if I have athlete’s foot?
No, but you should disinfect them. Spray the inside with antifungal spray or sprinkle antifungal powder daily. Let them air out for 24-48 hours between wears. Fungi survive in dark, damp shoes for months. Replace shoes only if they’re old, smelly, or visibly stained. Wearing breathable footwear and changing socks twice a day helps more than throwing things away.
Are there any side effects from antifungal creams?
Most people tolerate them well. But 22% of users report mild skin irritation - redness, stinging, or dryness. If it happens, stop using the cream for a day, then try again. If irritation persists, switch brands. Terbinafine is generally better tolerated than clotrimazole. Never use these creams on open wounds or near your eyes. If you develop swelling, hives, or blistering, stop immediately and see a doctor.
How long should I keep using antifungal cream after the rash disappears?
Continue for at least 1 week after the rash is gone. For tinea corporis, use it for a full 2-4 weeks. Fungi can still be alive under the skin even when it looks healed. Stopping early is the #1 reason ringworm comes back. Think of it like antibiotics - finish the course, even if you feel better.



paul walker on 30 January 2026, AT 01:27 AM
OMG I had ringworm on my elbow last year and I thought it was just dry skin-stupid me stopped the cream after 5 days. Came back worse. Now I’m that guy who treats everything like it’s ringworm. Even my cat side-eyes me when I grab the Lamisil.