QT Prolongation Risk Assessment Tool
Patient Assessment
Enter patient factors to determine risk of QT prolongation from antibiotics
Antibiotic Selection
Risk Assessment
Low RiskKey Safety Information
Critical Thresholds
QTc > 500 ms or increase > 60 ms from baseline requires immediate action.
Stop antibiotic immediately if these thresholds are exceeded.
Correcting Electrolytes
Correcting potassium to >4.0 mmol/L and magnesium to >2.0 mg/dL often reverses QT prolongation.
When you take an antibiotic like azithromycin or ciprofloxacin, you’re usually thinking about killing the infection-not your heart. But for some people, especially older adults or those on multiple meds, these common drugs can quietly mess with your heart’s rhythm. The problem? QT prolongation. It’s not something you feel. No chest pain. No dizziness. Just a delay in your heart’s electrical reset that can, in rare but deadly cases, trigger Torsades de Pointes-a chaotic, life-threatening arrhythmia.
Why Fluoroquinolones and Macrolides Are a Problem
Fluoroquinolones (like ciprofloxacin, levofloxacin, moxifloxacin) and macrolides (like erythromycin, clarithromycin, azithromycin) are both on the CredibleMeds® list of drugs known to prolong the QT interval. They do this by blocking the hERG potassium channel in heart cells. That channel is responsible for pulling the electrical charge back down after each heartbeat. Block it, and the repolarization phase drags on. The longer it takes, the higher the chance of dangerous rhythms. Not all drugs in these classes are equal. Moxifloxacin carries a higher risk than levofloxacin. Erythromycin is far riskier than azithromycin. This isn’t theoretical. A 2021 study tracking ICU patients on IV ciprofloxacin and erythromycin found measurable QT prolongation within hours of the first dose. In fact, sparfloxacin-the most dangerous fluoroquinolone-was pulled from the market in the 1990s for exactly this reason.Who’s at Risk?
It’s not just about the drug. It’s about the person taking it. Risk skyrockets when multiple factors pile up:- Age over 65
- Female gender (women have 2-3 times higher risk of TdP)
- Low potassium (<3.5 mmol/L) or low magnesium (<1.7 mg/dL)
- Heart disease-especially heart failure, low ejection fraction, or prior heart attack
- Other QT-prolonging drugs (antiarrhythmics, antidepressants, antifungals)
- Drugs that slow down antibiotic metabolism (like fluconazole or cimetidine)
- Existing long QT syndrome (genetic or acquired)
- Bradycardia (heart rate under 50 bpm)
- Chronic kidney disease
How QT Prolongation Is Measured
You can’t see QT prolongation without an ECG. But not all ECG readings are created equal. The key is correcting the QT interval for heart rate. Two formulas are used:- Bazett’s formula: QTc = QT / √RR - older, widely used, but overcorrects at fast heart rates and undercorrects at slow ones.
- Fridericia’s formula: QTc = QT / √RR³ - more accurate, especially for predicting mortality. It’s now the preferred method in guidelines from 2023 onward.
- QTc >450 ms in men
- QTc >470 ms in women
What to Do Before and During Treatment
Monitoring isn’t optional. It’s a safety net. Here’s what the British Thoracic Society and VUMC Antimicrobial Stewardship Program recommend:For Macrolides (like azithromycin or clarithromycin):
- Get a baseline ECG before starting treatment.
- Repeat the ECG one month after starting-especially if you’re on long-term therapy (e.g., for COPD or bronchiectasis).
- If QTc rises above 500 ms or increases by 60 ms, stop the drug immediately.
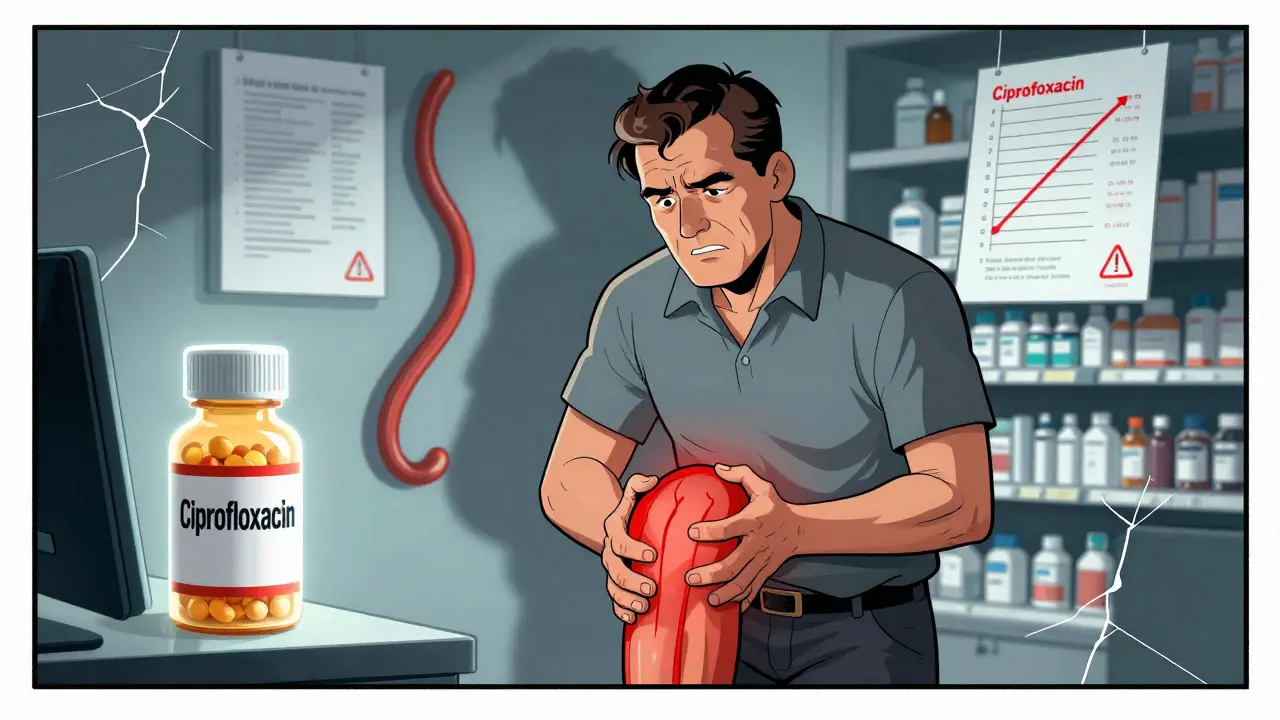
For Fluoroquinolones (like ciprofloxacin or levofloxacin):
- Check ECG 7-15 days after starting.
- Repeat monthly for the first 3 months.
- After that, periodic checks (every 3-6 months) if therapy continues.
- For high-risk patients, consider continuous telemetry during hospitalization.
When You Should Avoid These Drugs Altogether
Guidelines now strongly advise against using fluoroquinolones for uncomplicated UTIs-especially in women over 65 with multiple comorbidities. The risk of a fatal arrhythmia outweighs the benefit. Alternatives like nitrofurantoin or fosfomycin are safer and just as effective. Same goes for macrolides. If a patient is on a statin, an antipsychotic, or has low potassium, don’t reach for azithromycin or clarithromycin unless there’s no other option. Use a beta-lactam instead.
What to Do If QT Prolongation Is Found
If you spot QT prolongation:- Stop the antibiotic immediately if QTc >500 ms or increased >60 ms from baseline.
- Check electrolytes. Correct potassium to >4.0 mmol/L and magnesium to >2.0 mg/dL. This alone can reverse the risk.
- Discontinue any other QT-prolonging drugs if possible.
- Monitor continuously if the patient is symptomatic (palpitations, syncope, dizziness).
- Do not restart the drug-even at a lower dose. The risk doesn’t go away.
Real-World Pitfalls
Many clinicians still think: "It’s just a 10-day course. It won’t hurt." But TdP doesn’t need weeks. It can happen after the first dose. A 2005 review found 17 documented cases of levofloxacin-induced TdP-even in patients with no prior heart issues. Another trap? Misreading the ECG. Bundle branch blocks, paced rhythms, or wide QRS complexes (>140 ms) can make the QT look longer than it is. Always check the QRS duration. If it’s wide, the QT measurement is unreliable. And don’t forget: some patients are genetically predisposed. A family history of sudden cardiac death or unexplained fainting should raise red flags-even if the ECG looks normal.The Bigger Picture
Antibiotic stewardship isn’t just about preventing resistance. It’s about preventing harm. Fluoroquinolones and macrolides are overused. In 2025, the Canadian Network for Observational Drug Effect Studies (CNODES) found that nearly 40% of fluoroquinolone prescriptions in elderly patients had no clear indication. The FDA has issued multiple warnings. Hospitals are tightening protocols. But in outpatient clinics and nursing homes, the old habits die hard. The solution? Simple: Know your patient. Know their meds. Know their heart. Know their labs. And when in doubt, choose a safer antibiotic. Your patient’s heart will thank you.What is QT prolongation and why does it matter?
QT prolongation is a delay in the heart’s electrical recovery after each beat. When this delay gets too long, it can trigger Torsades de Pointes, a dangerous irregular heartbeat that can lead to sudden cardiac arrest. It’s silent-no symptoms until it’s too late. Antibiotics like fluoroquinolones and macrolides can cause it by blocking a key ion channel in heart cells.
Which antibiotics carry the highest risk of QT prolongation?
Among fluoroquinolones, moxifloxacin has the highest risk, followed by levofloxacin and then ciprofloxacin. Among macrolides, erythromycin is the riskiest, then clarithromycin, and azithromycin carries the lowest risk. Sparfloxacin was withdrawn due to extreme risk. Avoid these drugs if you have other risk factors.
How often should ECGs be done when taking these antibiotics?
For macrolides: baseline ECG before starting, then repeat at one month. For fluoroquinolones: first ECG 7-15 days after starting, then monthly for the first 3 months. After that, periodic checks every 3-6 months if therapy continues. High-risk patients may need continuous monitoring in hospital.
Is Bazett’s formula still the best way to calculate QTc?
No. Bazett’s formula (QTc = QT / √RR) overcorrects at high heart rates and undercorrects at low ones. Fridericia’s formula (QTc = QT / √RR³) is now preferred because it better predicts mortality and is more accurate across heart rate ranges. Most guidelines now recommend using Fridericia’s.
Can QT prolongation be reversed?
Yes-if caught early. Stopping the offending drug and correcting low potassium or magnesium levels often reverses the prolongation. But if Torsades de Pointes develops, it requires emergency treatment: magnesium sulfate, pacing, or isoproterenol. Prevention is far safer than treatment.
Are fluoroquinolones still used for UTIs?
No-not for uncomplicated UTIs, especially in older women. Guidelines now strongly recommend avoiding fluoroquinolones for simple urinary tract infections due to the risk of serious arrhythmias. Safer alternatives like nitrofurantoin or fosfomycin are just as effective and carry no cardiac risk.
What should I do if I’m on multiple medications?
Review all your meds with your doctor or pharmacist. Many common drugs-like antidepressants, antifungals, and statins-also prolong the QT interval. Combining them with fluoroquinolones or macrolides can be deadly. Ask: "Is this antibiotic necessary? Are there safer options?" Always get a baseline ECG before starting.

Michael Fitzpatrick on 23 November 2025, AT 04:13 AM
Man, I never realized how many of my old prescriptions could be quietly ticking time bombs for my heart. I was on azithromycin last year for a sinus infection and had no idea it could mess with my QT interval. I’m 58, on a statin, and my potassium’s always a little low-guess I got lucky. But now I’m gonna ask my doc for an ECG before any new antibiotic. Better safe than sorry, right?