Promethazine & Alcohol Risk Calculator
Calculate Your Risk
This tool estimates the combined sedative effects of promethazine and alcohol based on your specific situation.
Risk Assessment
Risk Level
Potential Symptoms
Recommended Actions
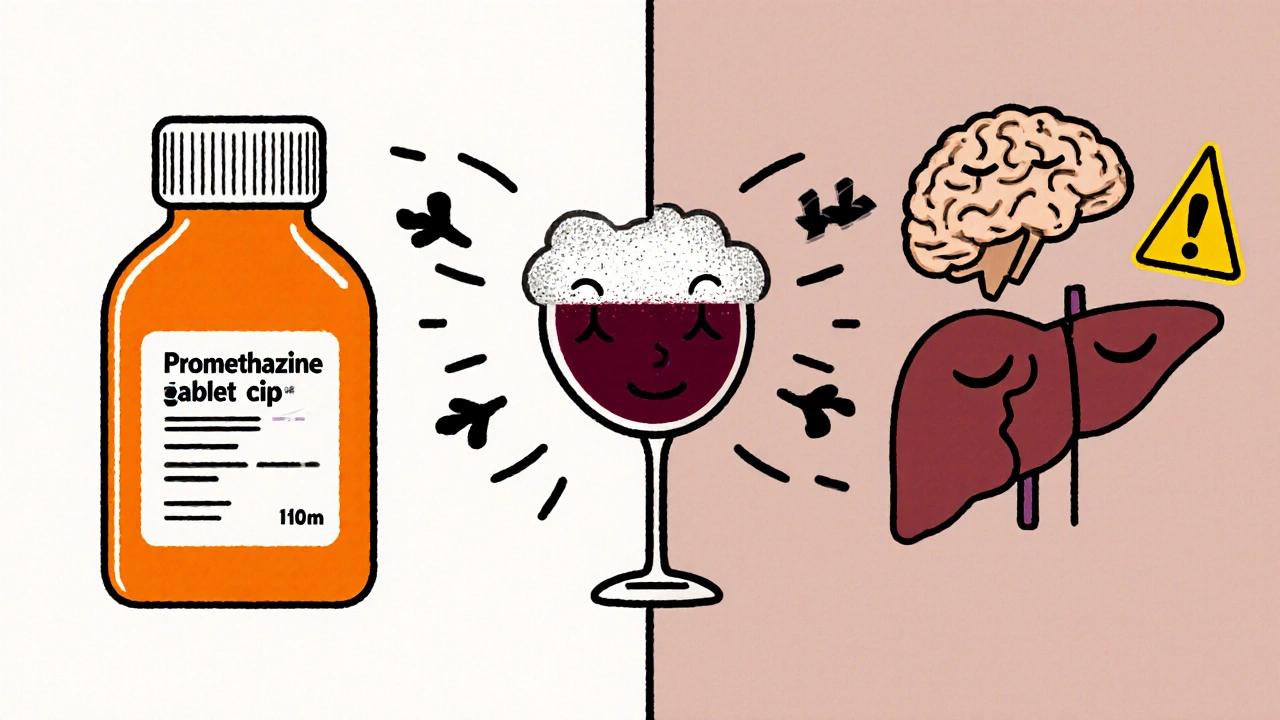
Mixing Promethazine and alcohol can be dangerous, especially if you’re not aware of how each substance affects the brain and body. Below we break down the chemistry, the short‑term dangers, and the long‑term health fallout so you can make an informed choice.
What is Promethazine?
Promethazine is an antihistamine that also acts as a sedative, anti‑nausea agent, and cough suppressant. It works by blocking histamine H1 receptors, which reduces allergy symptoms, and by dampening signals in the central nervous system (CNS) that trigger vomiting and wakefulness.
How Alcohol Affects the Body
Alcohol (ethanol) is a depressant that slows down brain activity, widens blood vessels, and impairs the liver’s ability to process toxins.
When you drink, ethanol enhances the activity of GABA, the main inhibitory neurotransmitter, and reduces glutamate, the primary excitatory messenger. This synergy creates the familiar feeling of relaxation - or, at higher doses, loss of coordination and judgment.
Why the Combination Is a Red Flag
The risky overlap comes from two major mechanisms:
- CNS depression: Both promethazine and alcohol suppress the brain’s arousal centers. When taken together, the effect isn’t just additive; it can become multiplicative, leading to profound sedation, slowed breathing, and impaired reflexes.
- Enzyme competition: Promethazine is metabolised primarily by the liver enzyme CYP2D6, which also processes ethanol’s by‑products. Alcohol can inhibit CYP2D6, causing promethazine levels to climb higher than intended.
Immediate Risks You Might Feel Tonight
- Respiratory depression - slowed breathing that can become dangerously shallow, especially in people with asthma or COPD.
- Extreme drowsiness - you may nod off in unsafe environments like driving or operating machinery.
- Reduced coordination - stumbling, slurred speech, and an increased chance of falls.
- Memory gaps - blackouts or fragmented recollection of the night’s events.
- Worsened nausea or vomiting - paradoxically, the anti‑nausea effect of promethazine can be blunted, leading to a cycle of puke‑and‑vomit.

Long‑Term Consequences If the Pattern Repeats
Occasional mishaps are alarming, but repeated mixing brings deeper health concerns.
- Liver disease - chronic alcohol consumption already taxes the liver; adding promethazine forces it to work overtime, raising the risk of hepatitis, fibrosis, or cirrhosis.
- Dependence - both substances can create psychological cravings; the body learns to expect the calming effect, which can evolve into a substance‑use disorder.
- Cardiovascular strain - promethazine can cause low blood pressure, while alcohol raises heart rate; the mismatch may trigger arrhythmias in vulnerable people.
- Persistent cognitive fog - long‑term CNS depression hampers memory formation and executive function.
Who Is Most at Risk?
Not everyone faces the same danger level. Pay close attention if you belong to any of these groups:
- Older adults - metabolism slows with age, making drug buildup more likely.
- People with pre‑existing liver conditions - reduced detox capacity magnifies toxicity.
- Patients already on sedatives, opioids, or other antihistamines - the combined depressant load can tip you over the edge.
- Individuals with sleep‑apnoea - decreased respiratory drive can trigger dangerous pauses in breathing.
Spotting an Overdose Early
If someone has taken promethazine and alcohol together and shows any of these signs, treat it as an emergency:
- Extreme drowsiness or inability to wake up.
- Blue‑tinged lips or fingertips (sign of low oxygen).
- Irregular or very slow breathing (less than 8 breaths per minute).
- Confusion, agitation, or hallucinations.
- Vomiting while unconscious - risk of choking.
Call emergency services immediately. If you’re trained, administer oxygen and be ready to perform CPR.

Safer Ways to Manage Symptoms
If you need an antihistamine or anti‑nausea aid, consider alternatives that carry less sedative weight:
- Loratadine or cetirizine - non‑sedating antihistamines that don’t amplify alcohol’s depressant effect.
- Ginger or acupressure bands for motion sickness - natural options with no CNS impact.
- Prescription anti‑nausea meds like ondansetron (if appropriate) - they work through serotonin pathways rather than histamine.
Always discuss medication changes with a healthcare professional, especially if you drink regularly.
Quick Reference Table
| Combination | Sedation Level | Respiratory Impact | Typical Use Cases |
|---|---|---|---|
| Promethazine + Alcohol | High | Significant (possible depression) | Allergy relief, nausea, sleep aid |
| Loratadine + Alcohol | Low | Minimal | Seasonal allergies |
| Cetirizine + Alcohol | Moderate | Low‑moderate | Allergy and hives |
What to Do If You’ve Already Mixed Them
Stop drinking immediately. Hydrate with water and avoid additional sedatives. If you feel unusually sleepy, have a friend stay with you, and keep a phone nearby in case you need to call for help.
Contact your doctor within 24 hours to discuss the episode. They can adjust your dosage, suggest safer alternatives, or provide a brief monitoring plan.
Frequently Asked Questions
Can a small amount of wine be safe with promethazine?
Even a single drink can amplify promethazine’s sedative push. If you must drink, keep the amount under one standard drink and stay under observation, but the safest route is to avoid alcohol altogether.
Does promethazine stay in the system longer if I drink?
Alcohol can slow the liver’s clearance of promethazine, extending its half‑life by up to 30 %. This means the drug’s effects linger longer, raising the chance of next‑day drowsiness.
Are there any over‑the‑counter antihistamines that won’t interact with alcohol?
Loratadine and fexofenadine are labeled as non‑sedating and have minimal interaction with alcohol. However, individual responses vary, so monitor how you feel.
What symptoms signal a dangerous drop in breathing?
Breathing slower than eight breaths per minute, shallow chest movements, or a bluish tint around lips or fingertips indicate hypoventilation and require immediate medical attention.
Can I take promethazine after a night of heavy drinking?
It’s best to wait at least 12 hours after heavy alcohol intake before retaking promethazine. This window lets the liver process most ethanol, reducing the risk of buildup.
Bottom line: the combination isn’t worth the gamble. Knowing how promethazine and alcohol interact equips you to avoid accidents, protect your liver, and keep your mind clear.


Brian Klepacki on 23 October 2025, AT 21:36 PM
Behold, the perilous tango of promethazine and booze-a duet destined for catastrophe! The very notion of blending a potent antihistamine with ethanol is akin to lighting fireworks in a fireworks factory. You might feel invincible for a fleeting moment, but the CNS depression creeps in like a silent assassin. Imagine your respiratory drive throttling down while your liver screams under the enzymatic overload. In short, it’s a theatrical tragedy waiting to unfold.