Transplant Medication Risk Calculator
This tool helps you understand how your specific health factors might influence immunosuppressant choices. It does NOT replace medical advice. Always consult your transplant team before making medication changes.
Your Medication Risk Assessment
Prograf (Tacrolimus)
Risk of kidney damage: 0%
Risk of blood sugar issues: 0%
Belatacept
Risk of kidney damage: 0%
Risk of lymphoma: 0%
Sirolimus
Risk of mouth sores: 0%
Risk of high cholesterol: 0%
Cyclosporine
Risk of hypertension: 0%
Risk of gum overgrowth: 0%
Personalized Recommendation
Based on your inputs, your transplant team might consider discussing [drug] as a potential alternative.
Important: This assessment is for informational purposes only. Your doctor will consider additional factors like your transplant type, age, and treatment history. Never change your medication without medical supervision.
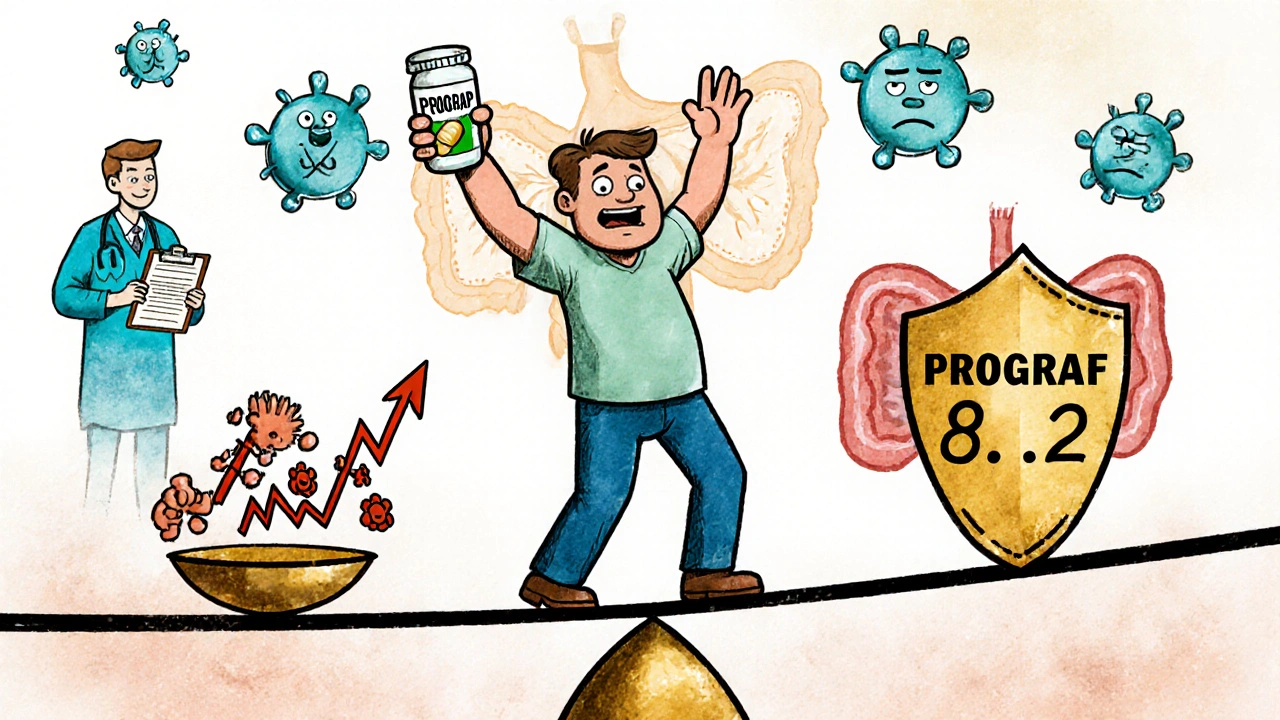
After a transplant, your body sees the new organ as a threat. That’s where Prograf (tacrolimus) comes in - it’s one of the most powerful tools doctors use to stop rejection. But it’s not perfect. Side effects like tremors, kidney strain, and high blood sugar can make life harder. Many patients wonder: are there better options? Or at least ones that fit their life better?
Why Prograf Is Still the Go-To
Prograf, the brand name for tacrolimus, has been the backbone of transplant care since the 1990s. It works by blocking T-cells - the immune system’s soldiers that attack foreign tissue. In clinical trials, patients on tacrolimus had significantly lower rates of acute rejection compared to older drugs like cyclosporine. A 2023 study in the American Journal of Transplantation found that kidney transplant patients on tacrolimus had a 22% lower rejection rate at one year than those on cyclosporine.
It’s not just about survival. Tacrolimus also helps organs last longer. For liver transplant patients, long-term graft survival is 85% at five years when tacrolimus is used as the main immunosuppressant. That’s why most transplant centers still start patients on it. But it’s a tightrope walk. Too much, and you risk kidney damage. Too little, and rejection kicks in.
Common Side Effects of Prograf
Prograf doesn’t just keep your immune system quiet - it affects your whole body. Common side effects include:
- Tremors in hands or feet
- High blood pressure
- Increased blood sugar (can trigger diabetes)
- Kidney function decline
- Nausea, headaches, insomnia
These aren’t rare. Up to 60% of patients report at least one of these within the first six months. Blood levels need constant monitoring - too high and you risk toxicity, too low and rejection can happen. Many patients end up switching not because the drug isn’t working, but because their body can’t handle the toll.
Alternative 1: Cyclosporine (Neoral, Sandimmune)
Cyclosporine was the first major immunosuppressant used after transplants. It’s older, cheaper, and still in use - especially in places where cost matters. But it’s less precise than tacrolimus.
Compared to Prograf, cyclosporine has higher rates of high blood pressure, gum overgrowth, and hair growth. It’s also harder on the kidneys long-term. However, it doesn’t raise blood sugar as much. For patients with prediabetes or a family history of diabetes, cyclosporine might be a safer pick.
Some centers use it in combination with lower-dose tacrolimus to reduce side effects. But overall, if you’re starting fresh after a transplant, most doctors won’t choose cyclosporine as the first-line drug anymore.
Alternative 2: Sirolimus (Rapamune)
Sirolimus works differently. Instead of targeting T-cells directly, it blocks a protein called mTOR - a key player in cell growth. This makes it useful for patients who need to avoid kidney damage or who’ve developed cancer after transplant.
It doesn’t harm the kidneys like tacrolimus does. In fact, some studies show it can help improve kidney function over time. It’s also linked to lower rates of skin cancer, which is a big concern for transplant patients on long-term immunosuppressants.
But sirolimus comes with its own problems: severe mouth sores, high cholesterol, poor wound healing, and fluid retention. It’s not used alone at first - usually added later if tacrolimus side effects become unmanageable. Patients need regular blood tests to monitor levels, and it takes weeks to reach steady state.
Alternative 3: Belatacept (Nulojix)
Belatacept is the newest major alternative. It’s an IV infusion given every few weeks, not a daily pill. It targets a different part of the immune system - the co-stimulation pathway - making it more selective than tacrolimus.
Studies show patients on belatacept have better kidney function after five years compared to those on tacrolimus. One trial found a 30% lower rate of chronic kidney damage. That’s huge for long-term survival.
But there’s a catch: it doesn’t work for everyone. About 10% of patients have a higher risk of post-transplant lymphoproliferative disorder (PTLD), especially if they’ve had Epstein-Barr virus. It’s also expensive and requires monthly clinic visits. Most transplant centers reserve it for patients who are young, healthy, and have no history of EBV.
Alternative 4: Mycophenolate Mofetil (CellCept) and Mycophenolic Acid (Myfortic)
These aren’t direct replacements for Prograf - they’re usually used alongside it. Mycophenolate blocks the production of DNA in immune cells, helping to keep the immune system in check without the same kidney or nerve side effects.
It’s commonly paired with low-dose tacrolimus to reduce the overall drug load. Many patients report fewer tremors and less high blood sugar when switching to a combo regimen. Side effects include diarrhea, nausea, and lower white blood cell counts.
Myfortic is the enteric-coated version of CellCept - designed to be easier on the stomach. If you’ve had GI issues with CellCept, Myfortic might be a better fit.
When to Consider Switching
You don’t switch just because you’re tired of pills. You switch when the trade-offs aren’t worth it. Here’s when a change makes sense:
- Your kidney function drops more than 25% in six months
- You develop new-onset diabetes after transplant
- Tremors or headaches interfere with work or sleep
- You’ve had skin cancer or precancerous lesions
- You can’t stick to daily dosing due to lifestyle or memory issues
Switching isn’t always easy. It takes weeks to adjust. Your doctor will monitor you closely - blood levels, kidney tests, and sometimes biopsies. Don’t change your meds without supervision. Even small changes can trigger rejection.

What About Generic Tacrolimus?
Many patients ask: can I just switch to the generic version of Prograf? The answer is yes - but with caution.
Generic tacrolimus is approved by the FDA and costs 70-80% less. But bioequivalence doesn’t mean identical. Some patients report side effects or rejection episodes after switching brands - even between different generics. That’s why most transplant centers stick with one brand for life.
If you must switch, do it under strict supervision. Get your blood levels checked within 72 hours. Don’t let a pharmacy change your prescription without your doctor’s approval.
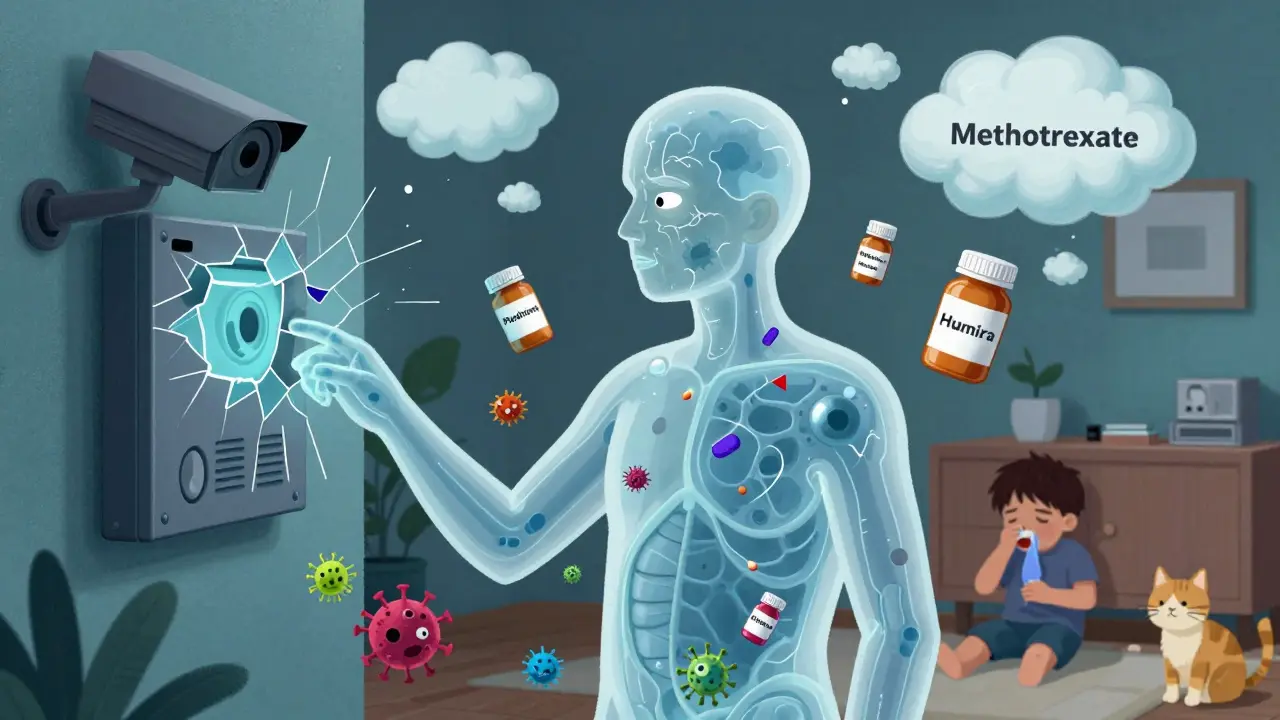
Personalizing Your Treatment
There’s no one-size-fits-all. Your ideal drug depends on:
- Type of transplant (kidney, liver, heart)
- Your age and overall health
- History of diabetes, kidney disease, or cancer
- Your ability to manage daily meds and clinic visits
- Insurance coverage and cost
For example: a 45-year-old kidney transplant patient with no diabetes and good kidney function might stay on tacrolimus. But a 60-year-old with early kidney damage and high blood sugar might benefit from switching to belatacept or adding sirolimus.
Some patients end up on a combo - low-dose tacrolimus + mycophenolate - to reduce side effects while staying protected. Others transition off tacrolimus entirely after a few years, once the risk of rejection drops.
What’s New in 2025?
Research is moving fast. New formulations of tacrolimus are being tested - once-weekly injections and slow-release capsules that keep levels stable without daily spikes. Early trials show promise in reducing side effects.
There’s also growing interest in personalized dosing using genetic testing. Some people metabolize tacrolimus faster than others due to variations in the CYP3A5 gene. Testing for this can help doctors start with the right dose, avoiding dangerous highs or ineffective lows.
And while biologics like belatacept are still expensive, biosimilars are expected to hit the market in 2026 - which could make them more accessible.
Can I stop taking Prograf if I feel fine?
No. Even if you feel great, stopping tacrolimus suddenly can cause your body to reject your new organ within days. Immunosuppression isn’t optional - it’s life-saving. Always follow your doctor’s instructions, even if you’re symptom-free.
Which alternative has the fewest side effects?
There’s no perfect drug. Sirolimus avoids kidney and nerve damage but causes mouth sores and high cholesterol. Belatacept is gentler on kidneys but requires IV visits and carries a small risk of lymphoma. The "fewest side effects" depends on your health history. Work with your transplant team to match the drug to your risks.
Is generic tacrolimus as good as Prograf?
Generic tacrolimus is FDA-approved and effective for most people. But because it’s a narrow-therapeutic-index drug, small differences in absorption can matter. Many transplant centers prefer to keep patients on the same brand for life to avoid instability. If you switch, get your blood levels checked within 72 hours.
Can I switch from Prograf to sirolimus without risk?
Switching isn’t risk-free. Sirolimus takes weeks to build up in your system. During that time, your immunosuppression drops, raising rejection risk. Doctors usually overlap the two drugs for 2-4 weeks and monitor closely. Never switch on your own.
How do I know if my current drug is working?
You won’t feel it - that’s the point. Your doctor checks blood levels, kidney function, liver enzymes, and sometimes does biopsies. Stable levels, normal organ function, and no signs of rejection mean your regimen is working. If your numbers drift, your doctor may adjust your dose or drug.
Next Steps
If you’re on Prograf and struggling with side effects, talk to your transplant team. Bring a list of your symptoms, your medication schedule, and any concerns. Ask about alternatives - not just drugs, but combinations, dosing changes, or new options in trials.
Don’t wait until things get worse. The best time to switch is before rejection or organ damage happens. With the right plan, you can stay protected - and feel better doing it.


Jim Allen on 30 October 2025, AT 08:58 AM
Prograf got me through my liver transplant but damn if my hands don’t shake like I’m trying to start a lawnmower in winter. Switched to sirolimus last year - mouth sores? Yeah. But no more sugar spikes. Worth it.