When you’re on antibiotics, your gut knows it. The good bacteria get wiped out along with the bad. That’s why so many people end up with diarrhea, bloating, or yeast overgrowth-not because the antibiotic failed, but because it didn’t discriminate. Probiotics can help. But if you take them at the wrong time, they’ll just die before they ever get a chance to work.
Why Timing Matters More Than You Think
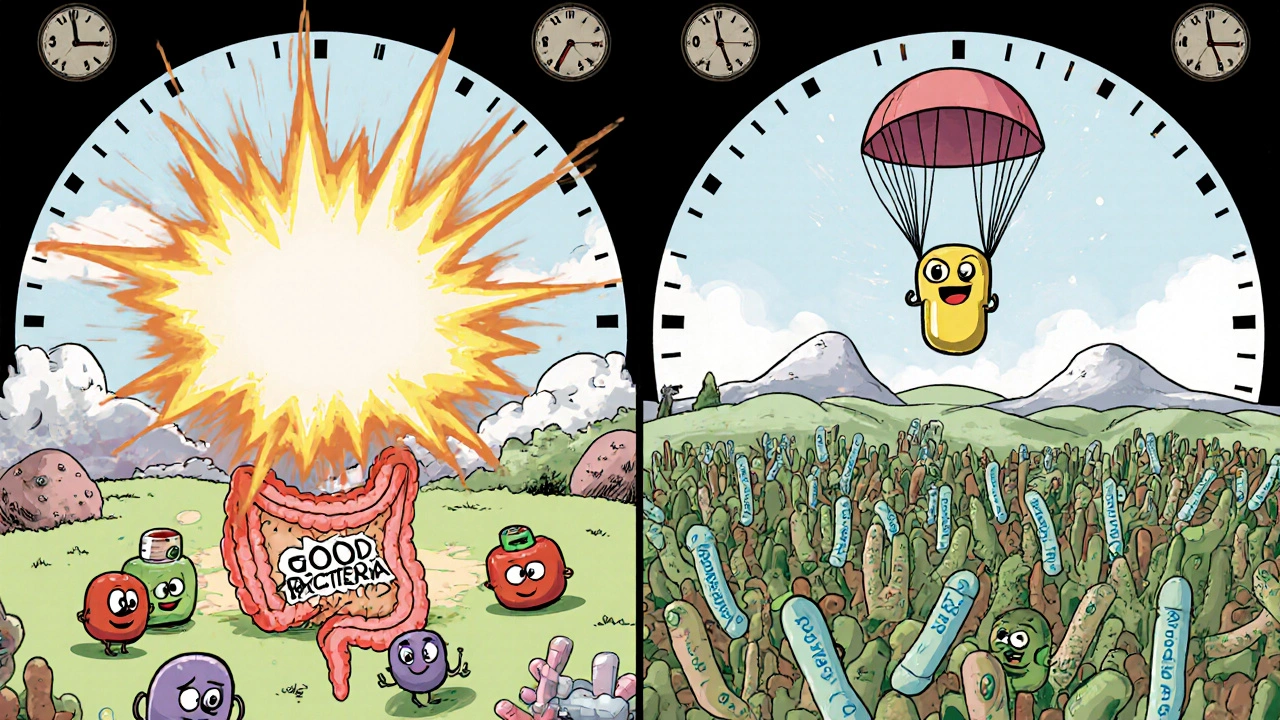
Antibiotics don’t pick and choose. They hit hard and fast, killing bacteria indiscriminately. If you swallow a probiotic capsule right after your amoxicillin, the live cultures inside will be destroyed before they even reach your colon. Studies show this reduces probiotic survival by 78% to 92%. That’s not just ineffective-it’s a waste of money and effort. The fix? Space them out. The gold standard is at least two hours between your antibiotic and your probiotic. This gives the antibiotic time to move through your stomach and upper intestine, so it’s no longer active in the lower gut when the probiotics arrive. It’s not magic-it’s basic pharmacokinetics.Which Probiotics Work Best?
Not all probiotics are created equal. Some survive antibiotics. Others don’t. Here’s what the science says:- Lactobacillus rhamnosus GG (LGG): Proven to cut antibiotic-associated diarrhea risk by nearly half. Best at 10-20 billion CFUs per day.
- Saccharomyces boulardii: A yeast, not a bacterium. This one doesn’t care about antibiotics. You can take it at the same time as your meds. It reduces diarrhea risk by 52% at 20 billion CFUs daily.
- Bifidobacterium strains: Also sensitive to antibiotics. Need the 2-hour buffer.
How Much Should You Take?
Dose matters. Too little, and you won’t see a difference. Too much, and you might just waste cash. Here’s what works based on real studies:- Mild cases (short course, no diarrhea): 5-10 billion CFUs per day
- Diarrhea or gut upset: 10-20 billion CFUs per day
- Long-term antibiotics (14+ days) or pre-existing gut issues: 20-40 billion CFUs per day
When to Stop Taking Them
Don’t quit as soon as the antibiotics run out. Your gut needs time to rebuild. The best studies show that continuing probiotics for 7 to 14 days after your last antibiotic pill leads to significantly better microbiome recovery. A 2024 study from Cymbiotika tracked 217 people on antibiotics. Those who stuck with probiotics for 14 days after treatment had an 89% recovery rate in their gut bacteria. Those who stopped early? Only 63%. That’s a huge difference.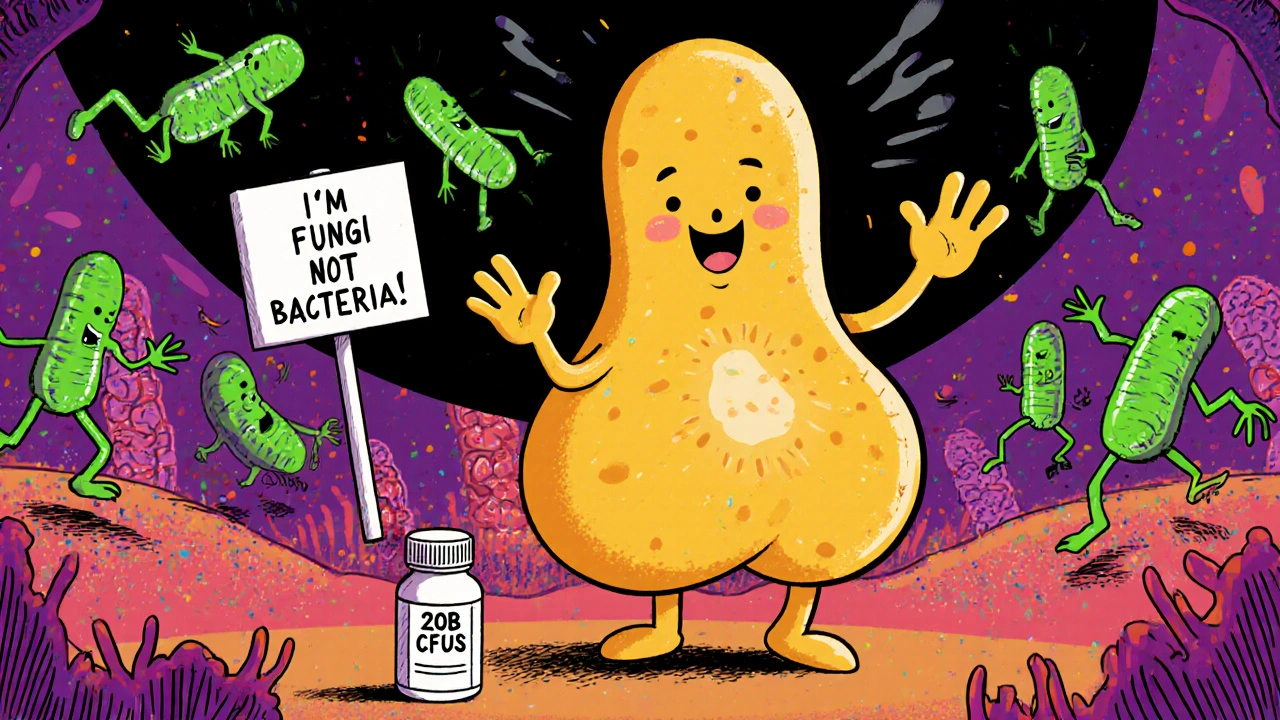
What About Saccharomyces boulardii? Can You Take It With Antibiotics?
Yes. And you should. Saccharomyces boulardii is a yeast. Antibiotics target bacteria, not fungi. That means this strain doesn’t get killed off. It can be taken at the same time as your meds without losing potency. It’s especially helpful for people prone to C. diff infections or severe diarrhea. In fact, the International Scientific Association for Probiotics and Prebiotics (ISAPP) specifically recommends it for concurrent use. No spacing needed. Just take it with your meal or your antibiotic-whichever is easier to remember.Real-Life Schedule Examples
Let’s say your doctor prescribed amoxicillin twice a day-at 8 a.m. and 8 p.m. If you’re using Lactobacillus or Bifidobacterium:- Take probiotic at 6 a.m. and 6 p.m.
- That’s two hours before each antibiotic dose.
- Take probiotic at 10 a.m. and 10 p.m.
- That’s two hours after each antibiotic.
What Most People Get Wrong
The biggest mistake? Taking probiotics at the same time as antibiotics. It’s tempting. You’re already swallowing pills. Why not add one more? But this is where most people fail. In vitro tests show that when taken together, up to 92% of the probiotic bacteria die before they can do anything. Another common error: stopping too soon. People think, “I feel better now, I don’t need these anymore.” But your gut isn’t healed just because the diarrhea stopped. The bacterial diversity is still low. That’s why continuing for 14 days after antibiotics is non-negotiable. And don’t assume all probiotics are equal. Only 32% of products on the shelf list the exact strain. Without knowing the strain, you can’t know if it’s effective. Look for LGG or S. boulardii on the label. If it’s not there, skip it.
What About Newer Probiotics With Time-Release Capsules?
Companies like Seed and Pendulum are developing acid-resistant, delayed-release capsules designed to survive antibiotics. Early data looks promising. Some of these formulations may eventually allow you to take probiotics with your meds without spacing. But as of November 2025, none have been proven in large-scale human trials to replace the 2-hour rule. The CDC’s 2024 antimicrobial resistance report confirms that 27 out of 31 major medical institutions still teach the 2-hour spacing protocol as standard care. Until more data comes in, stick with what works.When to Be Cautious
Not everyone needs probiotics during antibiotics. If you’re on a narrow-spectrum antibiotic like vancomycin (which targets mostly gram-positive bacteria), some experts believe the risk to your microbiome is lower. But this isn’t well studied. Don’t assume it’s safe to skip probiotics unless your doctor says so. Also, if you’re immunocompromised, talk to your doctor before taking any probiotic. While rare, yeast-based probiotics like S. boulardii can cause infections in people with severely weakened immune systems.Final Rule: Consistency Beats Perfection
You don’t need to be perfect. But you do need to be consistent. Missing doses cuts effectiveness by 37%, according to Seed’s 2023 study. If you forget to space them by an hour once? Don’t panic. Just take the probiotic when you remember, and get back on track. The goal isn’t flawless timing-it’s enough live bacteria surviving to make a difference. Two hours apart? Ideal. One hour? Better than nothing. Zero? You’re wasting your time.Bottom Line
Antibiotics are necessary. Probiotics can help you avoid the side effects. But only if you take them right.- Space bacterial probiotics at least two hours from antibiotics.
- Saccharomyces boulardii? Can be taken together-no spacing needed.
- Start within 48 hours of your first antibiotic dose.
- Continue for 7-14 days after finishing antibiotics.
- Use 10-20 billion CFUs of LGG or S. boulardii for best results.
- Check the label. If the strain isn’t listed, don’t buy it.
Can I take probiotics at the same time as antibiotics?
Only if you’re using Saccharomyces boulardii, a yeast-based probiotic. It’s not affected by antibiotics. For all bacterial probiotics like Lactobacillus or Bifidobacterium, taking them together kills up to 92% of the beneficial bacteria. Always space them at least two hours apart.
How long should I take probiotics after finishing antibiotics?
Continue for 7 to 14 days after your last antibiotic pill. Studies show that people who do this recover 89% of their gut bacteria diversity, compared to just 63% if they stop early. Your gut needs time to rebuild, even after symptoms disappear.
What CFU count should I look for in a probiotic?
For most people on antibiotics, 10-20 billion CFUs per day is the sweet spot. If you’re on a long course (14+ days) or have existing gut issues, go with 20-40 billion. Lower doses (5-10 billion) may help for short, mild courses, but higher doses are more reliable for preventing diarrhea.
Are multi-strain probiotics better than single-strain ones?
No. Research shows no significant advantage. A single strain like Lactobacillus rhamnosus GG or Saccharomyces boulardii is just as effective as products with 10 or 15 strains. Focus on proven strains, not marketing claims.
How do I know if my probiotic has the right strain?
Check the label. It must list the full strain name, like Lactobacillus rhamnosus GG or Saccharomyces boulardii CNCM I-745. If it just says “probiotic blend” or “10 billion CFUs” without the strain, it’s not backed by clinical data. Most products don’t disclose this-only 32% do.
Can I get probiotics from food instead of supplements?
Yogurt, kefir, and fermented foods contain probiotics, but they usually don’t have enough live cultures or the right strains to prevent antibiotic-associated diarrhea. Supplements are more reliable because they deliver a precise, tested dose. Food is great for maintenance, but not for fighting side effects during antibiotic treatment.
What if I forget to space my probiotic and antibiotic?
Don’t stress. If you accidentally take them together, just wait until the next scheduled dose and space them properly then. Missing one dose reduces effectiveness, but doesn’t ruin everything. Consistency over time matters more than perfection on a single day.
Do probiotics interfere with how antibiotics work?
No. There’s no evidence that probiotics reduce the effectiveness of antibiotics against harmful bacteria. Their job is to protect your gut, not fight infection. Taking them correctly helps prevent side effects without compromising treatment.

edgar popa on 13 November 2025, AT 04:56 AM
just took amoxicillin and a probiotic at the same time oops 😅 but hey i felt fine so maybe it’s all hype?