Steroid Risk Calculator
Personalized Risk Assessment
Personalized Risk Report
Overall Risk Level
Key Risk Factors
| Side Effect | Risk Level |
|---|---|
| Osteoporosis | |
| Adrenal Suppression | |
| Diabetes Risk | |
| Mood Changes | |
| Fluid Retention |
When you’re prescribed prednisone or prednisolone, it’s usually because something in your body is spinning out of control - maybe your immune system is attacking your joints, lungs, or skin. These drugs work fast. They quiet inflammation, calm allergic reactions, and stop autoimmune flare-ups in their tracks. But they come with a price tag written in side effects - some mild and temporary, others serious and lasting. The truth? Most people don’t realize how deep the risks go until they’re already on the medication. And by then, it’s too late to avoid them.
How Prednisone and Prednisolone Are the Same (and Why It Matters)
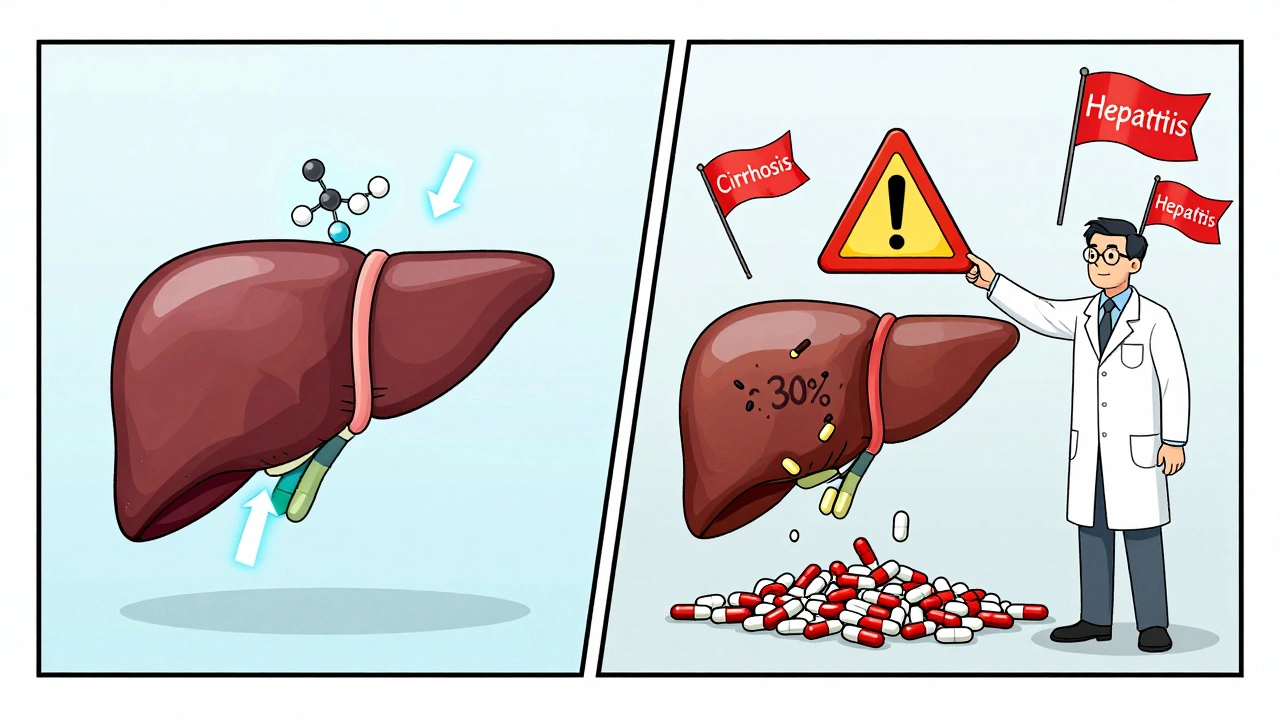
Prednisone and prednisolone aren’t two different drugs - they’re two versions of the same thing. Prednisone is a prodrug. That means your liver has to turn it into prednisolone before it can do its job. If your liver is healthy, this conversion happens smoothly. But if you have cirrhosis, hepatitis, or even just mild liver damage, your body might only convert 30% of the prednisone you take into the active form. That’s why doctors often switch patients with liver issues straight to prednisolone - no conversion needed.
For everyone else, 5 mg of prednisone equals 5 mg of prednisolone in effect. No difference in strength. No difference in how well they work. But there’s a tiny difference in how they hit your system. Prednisolone gets into your bloodstream about 1.8 times faster. That’s not usually a big deal - unless you’re a child with inflammatory bowel disease or someone who needs rapid control of a flare-up. In those cases, that speed can matter.
Short-Term Side Effects: What Happens in the First Few Weeks
If you’ve only been on these meds for a few days or weeks, you’re probably dealing with the short-term side effects. They’re annoying, sometimes scary, but usually go away once you stop.
- Insomnia - Nearly 7 out of 10 people report trouble sleeping. It’s not just being wired. Steroids mess with your cortisol rhythm, which controls your sleep-wake cycle. Taking your dose after 2 PM makes this worse. Taking it before noon cuts sleep problems in half.
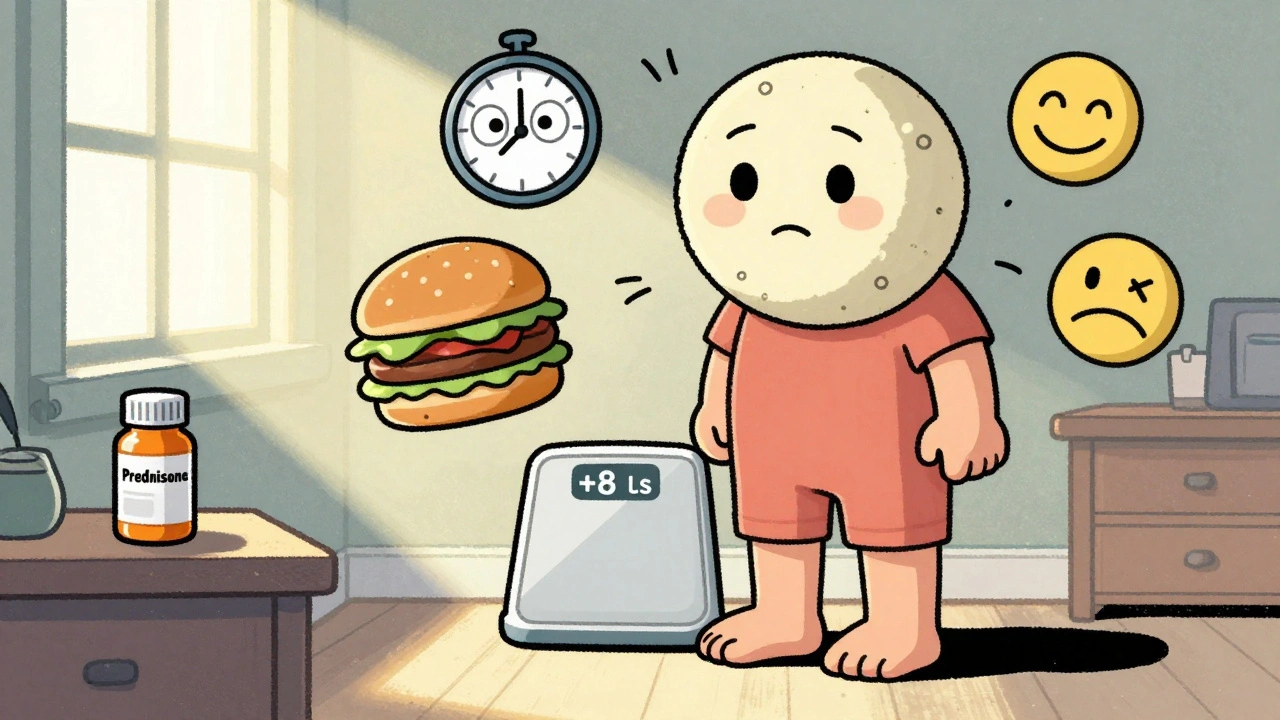
- Increased appetite and weight gain - You’re not lazy. You’re not weak. Your brain is being flooded with signals that tell you to eat. And your body starts storing fat around your belly and face. That’s why so many people get what’s called ‘moon face’ - the round, puffy cheeks.
- Mood swings - Some people feel euphoric. Others feel angry, anxious, or depressed. One Reddit user described calling 911 because he thought spiders were crawling all over his walls - at 60 mg, he was experiencing steroid psychosis. It’s rare, but it happens.
- Fluid retention and high blood pressure - Your body holds onto sodium like it’s gold. That means swelling in your ankles, bloating, and higher blood pressure. You might gain 5-10 pounds in a week just from water.
- Headaches and dizziness - Not always noticed, but common. Especially if your blood pressure spikes.
These effects hit hardest between days 3 and 10. That’s when your body is adjusting to the artificial flood of steroids. Most people feel better after a week or two - not because the side effects are gone, but because they get used to them. Don’t mistake that for safety.
Long-Term Side Effects: The Hidden Damage
Long-term use - meaning more than 3 weeks at a dose above 7.5 mg daily - changes everything. The risks aren’t just annoying anymore. They’re life-altering.
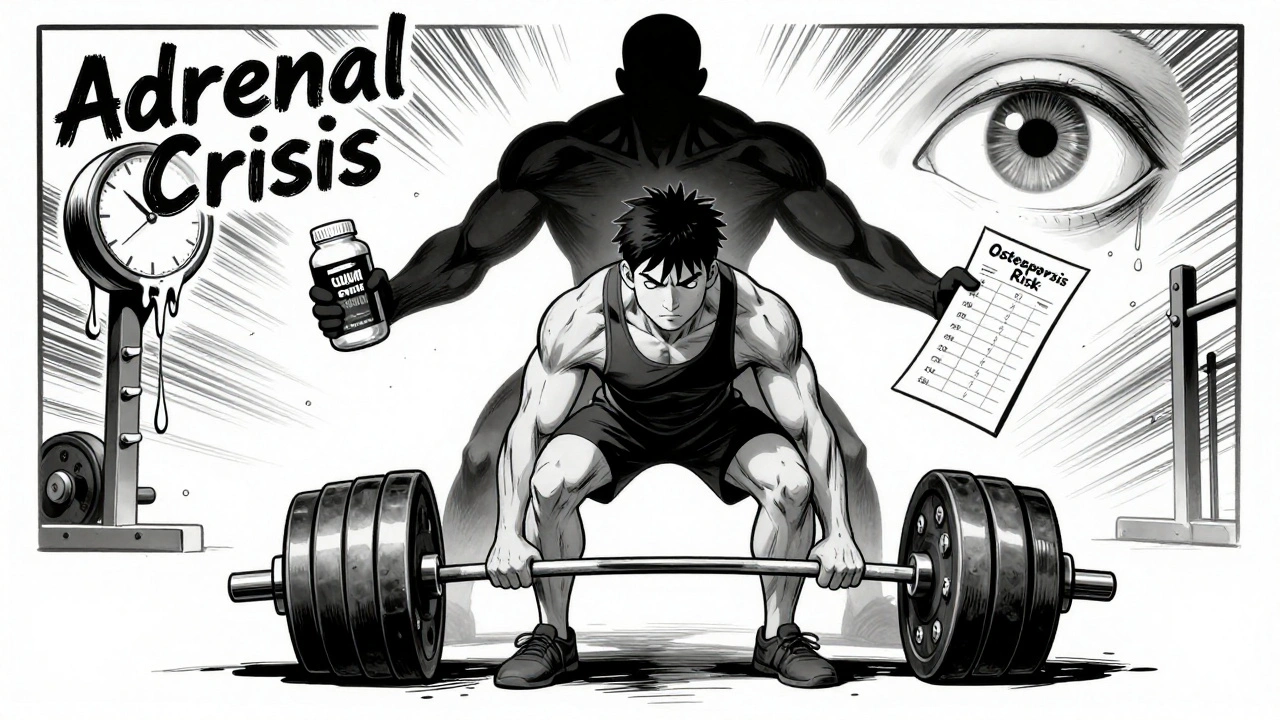
- Osteoporosis and bone fractures - Steroids stop your bones from rebuilding. After two years on these drugs, 63% of long-term users develop osteoporosis. One in three will break a bone - often from a simple fall or even sneezing. The risk goes up with every extra milligram and every extra month.
- Cataracts and glaucoma - Your eyes aren’t protected. About 41% of people on steroids for over a year need cataract surgery. Glaucoma risk rises too, especially if you’re over 40 or have a family history.
- Adrenal suppression - This is the silent killer. Your body stops making its own cortisol because the drug is doing it for you. If you stop suddenly, your adrenal glands can’t wake up fast enough. That’s adrenal crisis - low blood pressure, vomiting, confusion, even death. That’s why you never quit cold turkey. Tapering takes weeks, sometimes months.
- Diabetes and insulin resistance - Even if you’ve never had diabetes, steroids can push your blood sugar into the diabetic range. At doses above 20 mg daily, over half of non-diabetics develop steroid-induced hyperglycemia. That’s why doctors check your blood sugar every few weeks if you’re on long-term therapy.
- Muscle weakness and wasting - Your muscles start breaking down. You might find it hard to climb stairs or get up from a chair. This isn’t just aging. It’s steroid myopathy. It can take months to recover after stopping.
- Peptic ulcers and pancreatitis - Your stomach lining thins. Your pancreas gets inflamed. That’s why anyone on more than 5 mg daily for over 4 weeks gets a proton pump inhibitor like omeprazole to protect their gut.
- Avascular necrosis - This one is rare but devastating. Blood flow to your hip or shoulder joint dies. The bone collapses. You need surgery. It happens in 9-40% of people on high-dose steroids for more than three months.
These aren’t theoretical risks. They’re real. And they’re documented in patient registries, clinical trials, and years of medical records. The longer you’re on these drugs, the more your body forgets how to function without them.
Who’s Most at Risk?
Not everyone gets hit the same way. Some people sail through with minimal side effects. Others are wrecked by a 10-day course. Here’s who needs extra caution:
- Children - Growth slows by 1.2 cm per year for every 0.2 mg/kg/day of prednisolone. That’s not a small thing. Pediatricians monitor height every three months. Weight gain and delayed puberty are also common.
- Older adults - Bone loss happens faster. Blood pressure spikes are more dangerous. Muscle weakness increases fall risk. Even a short course can be risky.
- People with diabetes, high blood pressure, or liver disease - These conditions get worse fast on steroids. Your doctor needs to know your full history before prescribing.
- People with a history of mental health issues - Mood swings can turn into depression or psychosis. If you’ve had bipolar disorder, anxiety, or suicidal thoughts, steroids can trigger a crisis.
How to Protect Yourself
These drugs aren’t evil. They save lives. But they need to be handled like explosives - with respect, caution, and a plan.
- Take it early - Always take your dose before 2 PM. This helps your body’s natural cortisol cycle recover overnight.
- Watch your sodium - Keep salt under 2,000 mg a day. Eat more bananas, spinach, sweet potatoes - they’re high in potassium, which balances out the sodium retention.
- Move your body - Weight-bearing exercise (walking, lifting, stair climbing) cuts bone loss by 22%. Even 30 minutes a day helps.
- Take calcium and vitamin D - 1,200 mg calcium and 800-1,000 IU vitamin D daily is standard for anyone on steroids longer than 3 months. Your doctor should order a bone density scan after 6 months.
- Don’t skip doses - Missing a dose can trigger adrenal crisis. If you forget, call your doctor. Don’t double up.
- Never quit cold turkey - Tapering isn’t optional. It’s life-saving. Your doctor should give you a clear plan - often reducing by 1-2.5 mg every 1-2 weeks.
- Track your mood - If you feel unusually angry, anxious, or detached, tell your doctor. You’re not ‘overreacting.’ This is a known effect.
What About Alternatives?
There are no perfect replacements. Steroids are still the fastest, most reliable way to stop severe inflammation. But things are changing.
Biologics like tocilizumab and rituximab are now used in rheumatoid arthritis and lupus to reduce steroid dependence by up to 28%. New drugs called selective glucocorticoid receptor modulators are in trials - early results show they cut metabolic side effects by 60% while keeping the anti-inflammatory power. The FDA approved a new delayed-release prednisone in 2023 that lowers morning cortisol suppression and reduces mood swings by 32%.
But for now? If you need a steroid, it’s still prednisone or prednisolone. The goal isn’t to avoid them - it’s to use them smartly, for the shortest time possible, and with full awareness of what you’re signing up for.
Final Reality Check
Let’s be honest: most people don’t read the Medication Guide that comes with their prescription. They don’t know about the 63% osteoporosis rate or the 41% cataract risk. They just want the pain to stop.
And that’s okay. But you deserve to know the full picture. Prednisone and prednisolone are powerful tools. They’re not magic pills. They’re chemical interventions with deep, lasting consequences. The best outcome isn’t just symptom relief - it’s getting off them safely, with your bones, your eyes, your liver, and your mind still intact.
If you’re on these drugs now, talk to your doctor. Ask about your bone density. Ask about your blood sugar. Ask if you’re on the lowest possible dose. And if you’re about to start - ask if there’s another option. Don’t assume steroids are the only way. They’re the most common way. Not the only way.
Can prednisone and prednisolone be used interchangeably?
Yes, at equivalent doses - 5 mg of prednisone equals 5 mg of prednisolone in effect. But prednisone must be converted by the liver into prednisolone to work. If you have liver disease, your doctor may switch you to prednisolone directly, because your body can’t convert it efficiently. For most people with healthy livers, either works the same.
How long do short-term side effects last after stopping?
Most short-term side effects - like insomnia, increased appetite, mood swings, and fluid retention - start fading within 1-2 weeks after your last dose. Moon face and weight gain from water retention usually improve in 10-14 days. But full recovery of your natural cortisol production can take weeks to months, depending on how long you were on the drug.
Is it safe to take prednisone for just a few days?
Yes, a short course (5-10 days) at moderate doses is generally safe for most people. The risks of serious side effects like osteoporosis or adrenal suppression are very low at this duration. The benefits - like stopping a severe asthma attack or reducing swelling from an allergic reaction - usually far outweigh the temporary side effects. Always follow your doctor’s tapering plan, even for short courses.
What’s the lowest effective dose to minimize side effects?
The lowest effective dose is different for everyone, but experts agree: anything above 7.5 mg daily for more than 3 weeks increases the risk of serious side effects significantly. Many conditions can be managed with 5 mg daily or even less. Always ask your doctor if you can reduce your dose - even by 1 mg - and still stay in control. Lower is almost always better.
Do I need to take calcium and vitamin D if I’m on prednisone?
Yes, if you’re on prednisone or prednisolone for more than 3 months, you should take 1,200 mg of calcium and 800-1,000 IU of vitamin D daily. Steroids block bone formation and increase calcium loss. These supplements help slow bone loss, but they don’t eliminate the risk. Your doctor should also order a bone density scan after 6 months of use.
Can prednisone cause permanent damage?
Yes. Long-term use can cause permanent damage including osteoporosis with fractures, cataracts requiring surgery, adrenal insufficiency (meaning you’ll need lifelong hormone replacement), avascular necrosis of the hip or shoulder, and type 2 diabetes that doesn’t reverse after stopping. The earlier you stop, the better your chance of recovery - but some damage is irreversible.
Why do I feel so tired after stopping prednisone?
Your adrenal glands have been shut down by the drug and need time to restart cortisol production. This is called adrenal suppression. Fatigue, nausea, dizziness, and low blood pressure are common during withdrawal. That’s why tapering slowly is critical. If you stop too fast, you can go into adrenal crisis - a medical emergency. Give your body time to wake up. It can take weeks.
What Comes Next?
If you’re on prednisone or prednisolone, your next step isn’t to panic. It’s to get informed. Ask your doctor for a bone density test. Ask for a blood sugar check. Ask if you’re on the lowest possible dose. Ask if there’s a plan to get you off it.
These drugs aren’t the enemy. But they’re not harmless either. The goal isn’t to avoid them forever - it’s to use them like a scalpel, not a sledgehammer. Short. Precise. Controlled. And then, when you can, off.

Rupa DasGupta on 5 December 2025, AT 10:55 AM
I took prednisone for 2 weeks for a rash and woke up looking like a balloon animal 😅 my face was so puffy my dog didn’t recognize me. And the insomnia? I was wide awake at 3am thinking about spiders. Not joking. I swear I saw them crawling on the ceiling. My doctor just said "it’s normal" like that’s supposed to make me feel better. 🤦♀️