Imagine sitting across from your partner, watching their lips move, but the words just don’t come through. Not because they’re speaking softly-but because your own ears have stopped responding to low tones. That’s the quiet, creeping reality of otosclerosis, a condition where abnormal bone growth in the middle ear slowly steals your ability to hear-not with a bang, but a whisper.
What Exactly Is Otosclerosis?
Otosclerosis is not a tumor. It’s not an infection. It’s a glitch in bone remodeling. Normally, your bones renew themselves in a balanced way-old tissue breaks down, new tissue builds up. In otosclerosis, that balance breaks. Around the stapes bone, the smallest bone in your body (just 3.2mm long), bone starts growing where it shouldn’t. This extra bone fuses to the oval window, the tiny gate that connects your middle ear to the inner ear. When that happens, the stapes can’t vibrate. And without vibration, sound can’t travel properly to your cochlea.This isn’t just a theory-it’s measurable. Audiograms show an air-bone gap of 20-40 dB in most cases. That means sounds need to be much louder to reach your inner ear than they should. The result? Conductive hearing loss. You’re not deaf-you just can’t hear the lower pitches clearly. Voices sound muffled. The hum of the refrigerator? Gone. Your husband’s voice? Like he’s talking from another room.
Who Gets Otosclerosis and Why?
It’s not random. About 1 in 200 people in the UK have it. That’s over 300,000 people. And it’s not evenly spread. Women are twice as likely to develop it, especially between ages 30 and 45. If your mom or sister had it, your risk jumps significantly. Research has found 15 genetic links, with the RELN gene on chromosome 7 being the strongest. If you have a family history, you’re not just at risk-you’re in a high-risk group.Ethnicity matters too. People of European descent have the highest rates-0.3% to 0.4%. Asian populations are next, around 0.2%. African populations have the lowest, at about 0.1%. This isn’t just coincidence. It points to inherited biology, not environment.
And pregnancy? It can trigger or worsen otosclerosis. Hormonal changes seem to speed up the bone remodeling process. Many women first notice hearing loss during or right after pregnancy. That’s why doctors often ask about pregnancy history when evaluating young women with unexplained hearing loss.
How Is It Different From Other Hearing Problems?
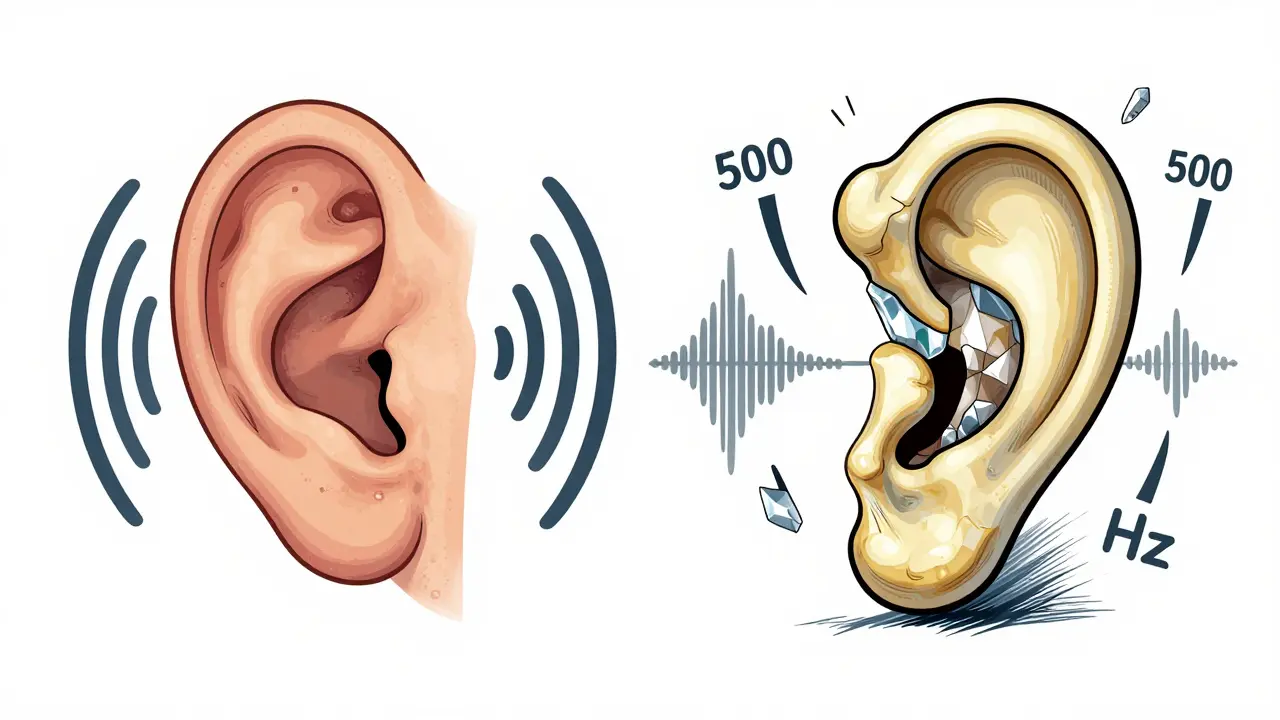
It’s easy to assume all hearing loss is the same. But otosclerosis has a signature pattern.Noise-induced hearing loss? That hits high frequencies first-think birdsong, alarms, or the ‘s’ and ‘th’ sounds in speech. Otosclerosis? It targets low frequencies. You’ll struggle to hear bass tones, men’s voices, or whispers. A 2022 study found people with otosclerosis often think their loved ones are mumbling-until their audiogram shows a 45 dB drop at 500 Hz.
Presbycusis (age-related hearing loss) usually starts after 65 and affects high tones. Otosclerosis hits decades earlier, often in your 30s or 40s.
Meniere’s disease comes with vertigo, ringing that comes and goes, and pressure in the ear. Otosclerosis? Steady, slow decline. No dizziness. Just fading sound.
And unlike some congenital ear problems, otosclerosis responds well to treatment. Surgery fixes the problem in 90-95% of cases. That’s higher than most other types of conductive hearing loss.
What Does It Feel Like to Live With It?
Real people describe it in ways medical reports can’t.One Reddit user, ‘MamaBear87,’ said she thought her husband was being rude-always mumbling-until her hearing test showed she couldn’t hear him below 500 Hz. Another, ‘HearingHope42,’ lost 30 dB of hearing in three years. Phone calls became impossible. She started relying on text messages just to keep up.
Tinnitus is common, too. Eighty percent of people with otosclerosis report ringing in the ears. For 35%, it’s bad enough to ruin sleep. That’s not just a side effect-it’s a second layer of suffering.
But there’s hope. One 45-year-old teacher in Tampa described her life after stapedectomy: ‘I can finally hear my students whispering in the back row.’ That’s not just improved hearing. That’s restored connection.
How Is It Diagnosed?
Your GP might miss it. Otosclerosis is often mistaken for Eustachian tube dysfunction-especially if you feel fullness in your ear. Studies show 22% of patients wait an average of 18 months before getting the right diagnosis.Here’s how it’s confirmed:
- Pure-tone audiometry: Shows a conductive hearing loss with an air-bone gap of at least 15 dB.
- Speech discrimination: Usually above 70%. This helps rule out inner ear damage.
- Temporal bone CT scan: Can reveal tiny radiolucent spots (0.5-2.0mm) near the oval window-early signs of abnormal bone growth.
There’s no blood test. No simple swipe. It’s all about the pattern of hearing loss and imaging. That’s why you need an ENT specialist-specifically one trained in otology. General audiologists may spot the loss, but only an otologist can confirm the cause.
Treatment Options: Hearing Aids or Surgery?
You have two main paths.Hearing aids are the first step for many. About 65% of people start here. They work well-especially for low-frequency loss. Modern digital aids can amplify specific frequencies without blasting everything else. But they don’t stop the bone growth. They just compensate.
Surgery is the only way to fix the root problem. The gold standard is stapedotomy. Instead of removing the entire stapes (stapedectomy), the surgeon makes a tiny hole in the footplate and inserts a prosthetic piston. This restores vibration. The procedure takes about an hour, is done under local or general anesthesia, and most people go home the same day.
Success rates? Around 90-95% for first-time surgeries. The air-bone gap closes to within 10 dB in most cases. That means normal hearing function returns. The StapesSound™ prosthesis, approved by the FDA in March 2024, uses a titanium-nitride coating to reduce scarring. Early results show 94% success at 12 months-better than older models.
But surgery isn’t risk-free. In about 1% of cases, patients lose hearing completely in the operated ear. That’s rare-but devastating. That’s why informed consent is non-negotiable. Your surgeon must explain this risk clearly.

What About Medications?
There’s no cure, but there’s a way to slow it down. Sodium fluoride, taken as a daily tablet, has shown promise. A 2024 double-blind study found it reduced hearing deterioration by 37% over two years compared to placebo. It doesn’t reverse the damage-but it can buy you time.It’s not for everyone. Fluoride can cause stomach upset. Your doctor will check your kidney function before prescribing it. But for someone who doesn’t want surgery yet-or can’t have it-it’s a real option.
What’s the Long-Term Outlook?
Without treatment, otosclerosis worsens. On average, hearing drops 15-20 dB over five years. That’s the difference between hearing a normal conversation and needing someone to shout.But with treatment? The outlook is excellent. Most people who get a stapedotomy regain near-normal hearing. Even those who choose hearing aids can live full, connected lives.
One concern? Fewer surgeons are doing these procedures. Since 2018, stapedectomies have dropped 15% annually. Younger otolaryngologists are focusing on cochlear implants and other high-tech areas. That means finding a skilled surgeon might take more effort. Ask for referrals. Look for someone who performs at least 10-15 stapedotomies a year.
What’s Next for Otosclerosis?
The future is getting personal. Researchers are developing polygenic risk scores-genetic profiles that can predict who’s likely to develop otosclerosis before symptoms start. Within five years, we may be able to screen high-risk individuals, monitor them closely, and intervene early.That’s not science fiction. It’s the roadmap from the American Hearing Research Foundation. And it’s why otosclerosis won’t disappear. It’s becoming more visible, more understood, and more treatable.
For now, if you’re noticing low-pitched sounds fading, especially if you’re a woman in your 30s or 40s with a family history-don’t wait. Get an audiogram. See an ENT. Don’t assume it’s just aging. Don’t assume it’s stress. It could be otosclerosis. And if it is? You have options. Real, effective ones.
Is otosclerosis hereditary?
Yes, otosclerosis often runs in families. About 60% of people diagnosed have a close relative with the condition. Genetic studies have identified at least 15 linked genes, with RELN on chromosome 7 being the most significant. If a parent has otosclerosis, your risk is higher-but not guaranteed.
Can otosclerosis cause total deafness?
No, otosclerosis rarely causes total deafness. It typically causes conductive hearing loss, which means sound doesn’t reach the inner ear properly-but the inner ear itself is usually still functional. In 10-15% of cases, it spreads to the cochlea and causes sensorineural loss, but even then, total deafness is extremely rare. With treatment, 90% of people regain functional hearing.
How do I know if I need surgery instead of hearing aids?
If your hearing loss is 30-40 dB or worse and you’re struggling with daily communication-like hearing conversations, watching TV, or using the phone-surgery is often recommended. Hearing aids help, but they don’t fix the underlying problem. Surgery restores natural hearing mechanics. Your ENT will compare your audiogram, speech scores, and lifestyle needs to help you decide.
What are the risks of stapedotomy?
The most serious risk is sudden, permanent sensorineural hearing loss in the operated ear-this happens in about 1% of cases. Other risks include dizziness (usually temporary), taste changes (due to nerve proximity), and tinnitus flare-ups. Revision surgeries have lower success rates (around 75%) than first-time procedures. Choosing an experienced surgeon reduces these risks significantly.
Can otosclerosis get worse after surgery?
The surgery fixes the stapes problem, so the conductive loss doesn’t return. But if the disease spread to the cochlea before surgery, that sensorineural loss can still progress slowly over time-about 0.5-1.0 dB per year. That’s why some patients still need hearing aids after surgery, especially for high-frequency sounds. Sodium fluoride may help slow this progression.
Are hearing aids effective for otosclerosis?
Yes, hearing aids are very effective for otosclerosis, especially for low-frequency loss. Modern digital aids can be programmed to boost only the frequencies you struggle with, leaving others unchanged. Many people use them successfully for years. They’re non-invasive and reversible. But they don’t stop the bone growth-only compensate for it.
How long does recovery take after stapedotomy?
Most people return to light activities within a week. Full recovery takes 4-6 weeks. You’ll avoid heavy lifting, flying, and getting water in your ear during this time. Hearing improvement often starts within days, but it can take up to 3 months to stabilize as the inner ear adjusts. Follow-up audiograms at 1 and 6 months are standard.
Can otosclerosis affect both ears?
Yes, it often does. About 70-80% of people with otosclerosis develop it in both ears, though usually not at the same time or to the same degree. One ear may be significantly worse. Surgery is typically done on the more affected ear first. If the other ear worsens later, a second procedure is possible.


Louis Paré on 30 December 2025, AT 09:49 AM
This whole post reads like a pharmaceutical ad disguised as medical advice. Stapedotomy? Sure, 95% success rate-until you’re the 1% who wakes up deaf. And don’t get me started on sodium fluoride. You’re literally poisoning your kidneys to delay a condition that’s not even fatal. Who’s funding this? Audiotech corporations? The ENT lobby? Wake up.