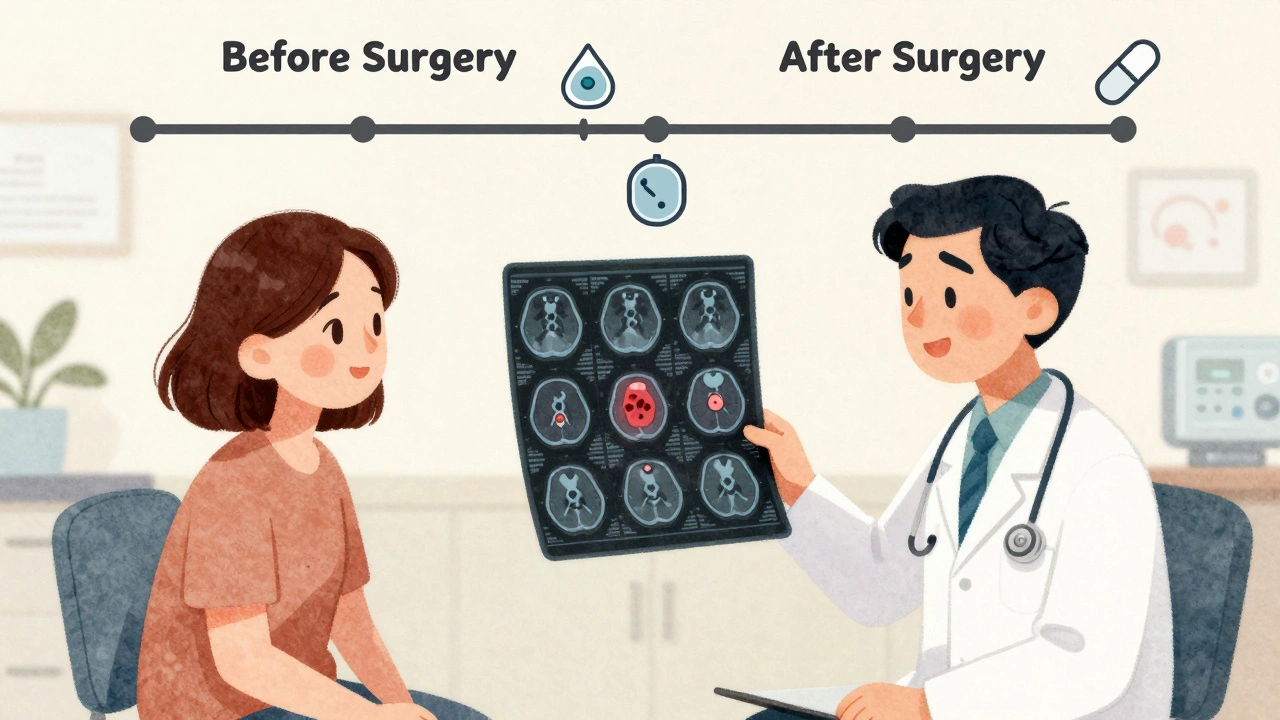
When you’re facing a cancer diagnosis, one of the first big decisions isn’t about which drug to take-it’s about when to take it. Should treatment come before surgery to shrink the tumor? Or after, to clean up what’s left? This isn’t just a technical detail. It’s a turning point in your care plan. For many cancers-especially lung and breast cancer-the answer isn’t one-size-fits-all. It depends on the tumor, the patient, and what the science now says about timing.
What Neoadjuvant Therapy Really Means
Neoadjuvant therapy means treatment before surgery. It’s not just about making the tumor smaller. It’s about testing how your cancer responds to drugs while it’s still inside your body. That’s something you can’t do with surgery alone. If the tumor shrinks dramatically after a few rounds of chemo or immunotherapy, that tells your doctors something powerful: the drugs are working. And if they’re working, your chances of long-term survival go up. In non-small cell lung cancer (NSCLC), for example, the CheckMate 816 trial showed that combining nivolumab (an immunotherapy) with chemotherapy before surgery led to a 24% pathologic complete response rate-meaning no live cancer cells were found in the removed tissue. Compare that to just 2.2% with chemo alone. That’s not a small difference. It’s life-changing. And patients who reached this level of response had a 37% lower risk of their cancer coming back or spreading within the first few years. For breast cancer, especially triple-negative or HER2-positive types, neoadjuvant therapy is now standard for many patients. About 35% of women with stage II or III breast cancer in the U.S. now get treatment before surgery. If they achieve a pathologic complete response (pCR), their survival rates jump significantly. In fact, pCR has become one of the strongest predictors of long-term outcomes in these subtypes.What Adjuvant Therapy Does
Adjuvant therapy comes after surgery. Its goal is simple: kill any cancer cells that might still be hiding in your body, even if scans look clean. These are the cells too small to see, too few to detect-but dangerous enough to cause recurrence later. For decades, this was the default. Remove the tumor, then hit it with chemo or radiation to be safe. But as we’ve learned more about how tumors behave, we’ve realized something important: if the cancer is resistant to treatment, giving drugs after surgery doesn’t always help. And if the drugs are effective, why wait? Why not start them earlier? In lung cancer, adjuvant immunotherapy became FDA-approved after CheckMate 816 showed benefit from pre-surgery treatment. But here’s the twist: newer data suggests the extra round of immunotherapy after surgery might not add much benefit-and it adds more side effects.The Real Difference: Seeing the Response
The biggest advantage of neoadjuvant therapy isn’t survival-it’s information. When you treat before surgery, you get real-time feedback. Did the tumor shrink? Did it disappear? Did your body handle the drugs well? That feedback shapes everything that comes next. If you have a strong response, your oncologist might decide you don’t need as much post-surgery treatment. If there’s little to no response, they can switch gears quickly. Maybe try a different drug combo. Maybe enroll in a clinical trial. Maybe avoid surgery altogether if the cancer is too aggressive. With adjuvant therapy, you don’t get that insight. You give the drugs after the fact, hoping they worked. You’re guessing. A 2024 meta-analysis in JAMA Network Open looked at over 3,200 patients with resectable lung cancer across four major trials. It found no significant survival difference between those who got immunotherapy only before surgery and those who got it before and after. But the group that got both had nearly twice as many serious side effects-29.8% versus 17.6%. That’s not a trade-off worth making if the outcome is the same.When Adjuvant Therapy Still Makes Sense
That doesn’t mean adjuvant therapy is outdated. It still has its place. For patients whose tumors don’t respond well to neoadjuvant treatment, post-surgery therapy can be critical. In breast cancer, if a patient doesn’t reach pCR after neoadjuvant chemo, adding extra drugs like capecitabine can reduce recurrence risk. Also, for some patients, surgery needs to happen right away. If the tumor is causing pain, blocking an airway, or pressing on vital organs, waiting weeks for neoadjuvant therapy isn’t safe. In those cases, surgery first, then treatment, is the better choice. And then there’s the human factor. Some patients are terrified of waiting. They want the tumor out now. They don’t want to sit for 12 weeks with cancer still inside them, wondering if it’s growing. That fear is real. And it matters.
Who Gets Neoadjuvant Therapy? It’s Not for Everyone
The National Comprehensive Cancer Network (NCCN) recommends neoadjuvant chemoimmunotherapy for stage IB (tumors 4 cm or larger) through stage IIIA non-small cell lung cancer. For breast cancer, it’s standard for:- Triple-negative breast cancer (TNBC)
- HER2-positive breast cancer
- Stage II or III hormone receptor-positive cancer where downsizing helps with breast-conserving surgery
How Timing Works in Practice
Neoadjuvant therapy usually lasts 3 to 4 cycles, delivered over 9 to 12 weeks. After that, surgery is scheduled 3 to 6 weeks later. Why the wait? Your body needs time to recover from the drugs. Giving surgery too soon increases the risk of complications like poor wound healing or infection. After surgery, if your doctor recommends adjuvant therapy, it typically runs for another 4 to 6 months. But here’s the new thinking: if you already had immunotherapy before surgery, do you really need more after? The evidence says maybe not. A 2023 survey of 257 community oncologists showed that 78% now offer neoadjuvant immunotherapy for stage II-III lung cancer-up from just 42% in 2021. That’s a massive shift in just two years. It’s not just academic. It’s happening in clinics across the country.What’s Changing Right Now
The field is moving fast. In 2022, the FDA approved neoadjuvant nivolumab plus chemo for resectable lung cancer-and then approved adjuvant nivolumab after surgery. But now, trials like KEYNOTE-867 are testing whether the adjuvant part is even necessary. Meanwhile, circulating tumor DNA (ctDNA) testing is emerging as a game-changer. After surgery, a simple blood test can detect if cancer DNA is still floating in your bloodstream. If it is, you likely need more treatment. If it’s not, you might be able to avoid it entirely. Twelve clinical trials are already exploring this approach. The goal? Personalized sequencing. Not just “before or after.” But “how much, for whom, and when.”
What Patients Are Saying
On cancer forums, stories vary. One lung cancer patient wrote: “I got neoadjuvant nivolumab. My tumor shrank so much, the surgeon said he could remove it with less damage. I had a 90% pathologic response. That gave me hope.” Another breast cancer patient said: “I chose adjuvant chemo because I didn’t want to wait. But later, I learned I might have benefited from knowing how my tumor responded before surgery. I wish I’d known more.” A 2023 survey by the Lung Cancer Alliance found 62% of patients on neoadjuvant therapy felt anxious during the waiting period before surgery. That’s understandable. But 78% of those same patients also said they’d choose it again, because they felt more in control.What You Should Ask Your Doctor
If you’re facing surgery for lung, breast, or another solid tumor, here are five questions to ask:- Is neoadjuvant therapy an option for my type and stage of cancer?
- What’s the chance my tumor will respond? Do we know my tumor’s biomarkers (like PD-L1 or HER2)?
- What are the risks of waiting for surgery? Could my cancer grow during treatment?
- Will I need additional treatment after surgery? What’s the evidence for that?
- Can we test for circulating tumor DNA after surgery to guide next steps?

Gillian Watson on 4 December 2025, AT 10:27 AM
I’ve seen this play out with my sister-neoadjuvant therapy gave her a shot at breast-conserving surgery when she thought she’d lose everything. The waiting was hell, but knowing the drugs worked before they cut? That’s peace of mind you can’t buy.Also, side effects dropped for her after surgery because they cut the adjuvant dose. Just saying.