Every year, over 200,000 adverse events linked to sedatives and opioids happen in U.S. healthcare settings. Seniors make up 65% of the cases where breathing stops during sedation. Why? Because their bodies process drugs differently. Their liver and kidneys don’t work as fast. Their brain becomes more sensitive. A dose that’s safe for a 40-year-old can push an 80-year-old into respiratory arrest-sometimes without warning.
Why Seniors Are at Higher Risk
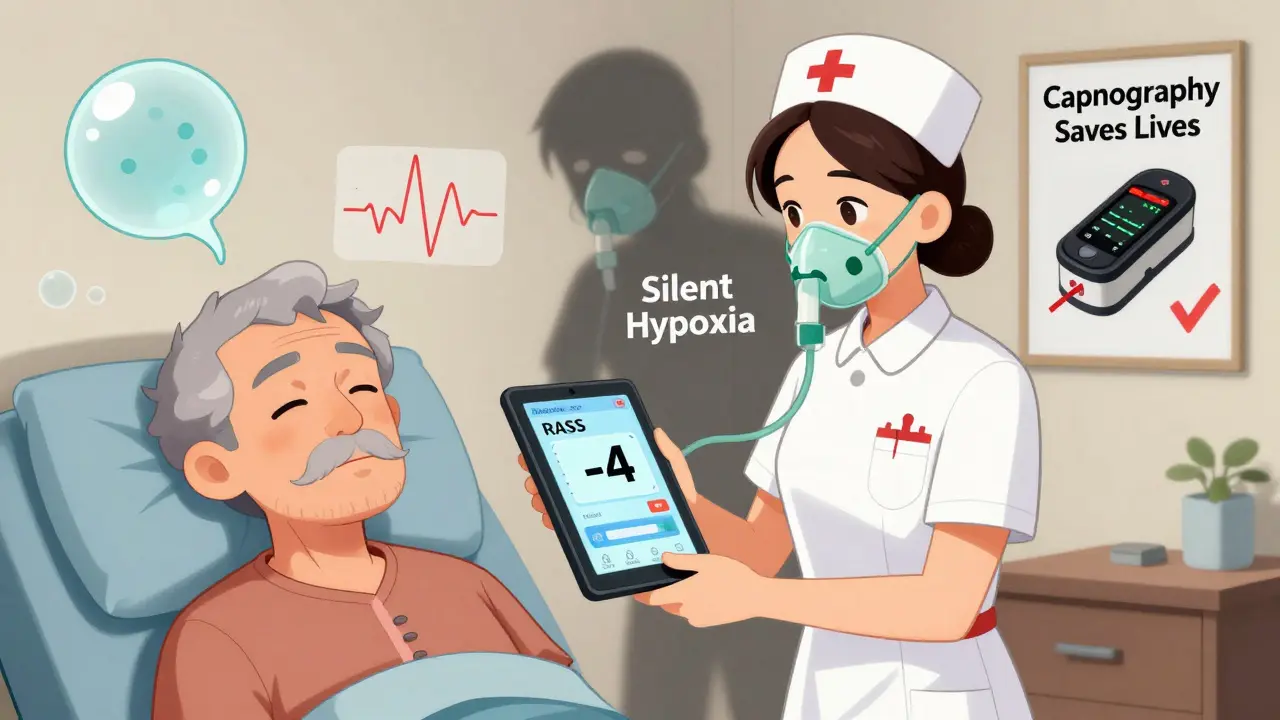
A 75-year-old patient taking 5 mg of midazolam for a colonoscopy isn’t just getting the same dose as a 30-year-old. Their body metabolizes drugs 30-50% slower. Their kidneys clear medications at a rate that drops 0.8 mL/min/1.73m² every year after 40. Even their blood-brain barrier becomes more porous, letting more drug reach the brain. This isn’t about being ‘fragile.’ It’s about biology. And when you combine that with chronic conditions like COPD or heart failure-common in older adults-the risk multiplies.One of the most dangerous myths is that if someone’s oxygen level looks fine, they’re safe. But when seniors are on supplemental oxygen, their SpO2 can stay above 94% even while they’re barely breathing. This is called ‘silent hypoxia.’ By the time their oxygen drops, they’re already in trouble. That’s why relying on pulse oximetry alone is like driving with only a fuel gauge and no speedometer.
What to Watch For: The Key Signs of Over-Sedation
You don’t need fancy equipment to spot early warning signs. But you do need to know what to look for-and when to act.- Respiratory rate below 8 breaths per minute: This is the most reliable red flag. Even if oxygen looks good, slow breathing means carbon dioxide is building up.
- Unresponsiveness: If the person doesn’t respond to a gentle shake or their name being called, they’re too sedated. Use the Richmond Agitation-Sedation Scale (RASS). A score of -2 or lower means moderate to deep sedation. At -4 or -5, they’re unarousable. That’s an emergency.
- Shallow or irregular breathing: Look for chest movement. Is it weak? Is there long pauses between breaths? That’s not normal.
- Low blood pressure: Systolic pressure below 90 mmHg can mean the body is shutting down. This often follows respiratory depression.
- Slowed heart rate: Below 50 bpm in a senior not on beta-blockers is a warning sign. It often happens as oxygen drops and the brain triggers a vagal response.
These signs don’t always show up together. That’s why you need to monitor multiple things at once.
Monitoring Tools That Save Lives
The gold standard isn’t one tool-it’s a combination. The American Society of Anesthesiologists (ASA) says continuous multimodal monitoring is non-negotiable for seniors.Capnography: The Silent Hero
Capnography measures carbon dioxide in exhaled breath. It’s the only tool that tells you if someone is actually breathing-not just oxygenating. In seniors, it detects apnea (no breathing) with 92% accuracy. Pulse oximetry? Only 67%. That’s a huge gap.Here’s why it matters: A 2020 study of 387 seniors found that 40% of those on oxygen had dangerous hypoventilation that pulse oximetry missed. Capnography caught it. And it does it 12-14 minutes before oxygen levels drop. That’s enough time to reverse the overdose before it becomes fatal.
But capnography has a flaw: false alarms. Irregular breathing patterns in elderly patients trigger alarms 38% of the time. That’s why you can’t rely on it alone. You need to pair it with other tools.
Integrated Pulmonary Index (IPI)
The IPI is a smart algorithm that takes four readings-oxygen saturation, respiratory rate, heart rate, and CO2-and turns them into a single number from 1 to 10. A score below 7 means trouble. In a 2021 study of 1,245 seniors, the IPI predicted respiratory compromise 12.7 minutes before oxygen dropped. One nurse on Reddit shared how her 82-year-old patient’s IPI dropped to 5.2 during a colonoscopy. She stopped the procedure, reversed the sedation, and avoided a respiratory arrest.Respiratory Volume Monitoring (RVM)
RVM uses bioimpedance to measure actual air volume moving in and out of the lungs. It’s even better than capnography at catching early hypoventilation-14.3 minutes before pulse oximetry alarms. But it’s tricky. The electrodes can irritate fragile senior skin, and 22% of placements fail because of thin, dry skin or movement. If you use it, use hydrocolloid dressings under the electrodes. That cuts skin injuries by 67%.Level of Consciousness: RASS Scale
Never guess if someone is ‘just sleepy.’ Use the Richmond Agitation-Sedation Scale. It’s simple:- +1 to +4: Agitated
- 0: Alert and calm
- -1 to -2: Light sedation
- -3: Moderate sedation
- -4: Deep sedation
- -5: Unarousable
Any score below -2 means you need to act. Don’t wait for the patient to stop breathing. At -3, reduce or stop the sedative. At -4 or -5, reverse with naloxone if opioids are involved.
What Not to Do
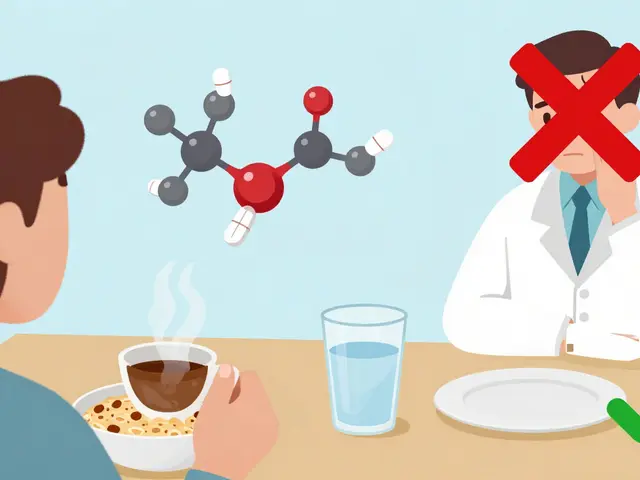
There are common mistakes that lead to disasters.- Don’t use adult dosing for seniors. A 2023 report found 42% of facilities still give the same sedative dose to a 78-year-old as to a 45-year-old. That’s dangerous. Use this formula: Adjusted dose = standard dose × (1 - 0.005 × (age - 20)). For a 75-year-old, that’s about 67% of the standard dose.
- Don’t skip capnography. Even if the patient ‘looks fine.’ The 2021 Massachusetts General Hospital case involved a 90-year-old who died during a PEG tube placement because staff only checked oxygen every 10 minutes. They missed 14 minutes of apnea.
- Don’t assume ‘normal’ vital signs are safe. A senior’s ‘normal’ heart rate might be 55. That’s okay. But if it drops from 55 to 42? That’s a problem. Look for trends, not just numbers.
- Don’t rely on intermittent checks. Checking every 5 minutes misses 78% of respiratory events. Continuous monitoring isn’t optional-it’s the standard.
What Works: Real-World Success Stories
The Mayo Clinic implemented a protocol in 2022 combining RASS scoring with continuous capnography for patients over 75. Result? A 41% drop in oversedation events. No deaths. No arrests. Just better care.Hospitals that use the IPI algorithm report fewer false alarms and faster responses. Nurses say they feel more confident. Patients feel safer.
Even outpatient centers are catching up. The FDA cleared the Opioid Risk Monitoring System (ORMS) in May 2023. It’s a device that links IV pain pumps to capnography and pulse oximetry. If breathing slows below 8 breaths per minute, it automatically pauses the opioid drip. In a 2022 trial, it cut respiratory depression in seniors by 58%.
What You Need to Do Today
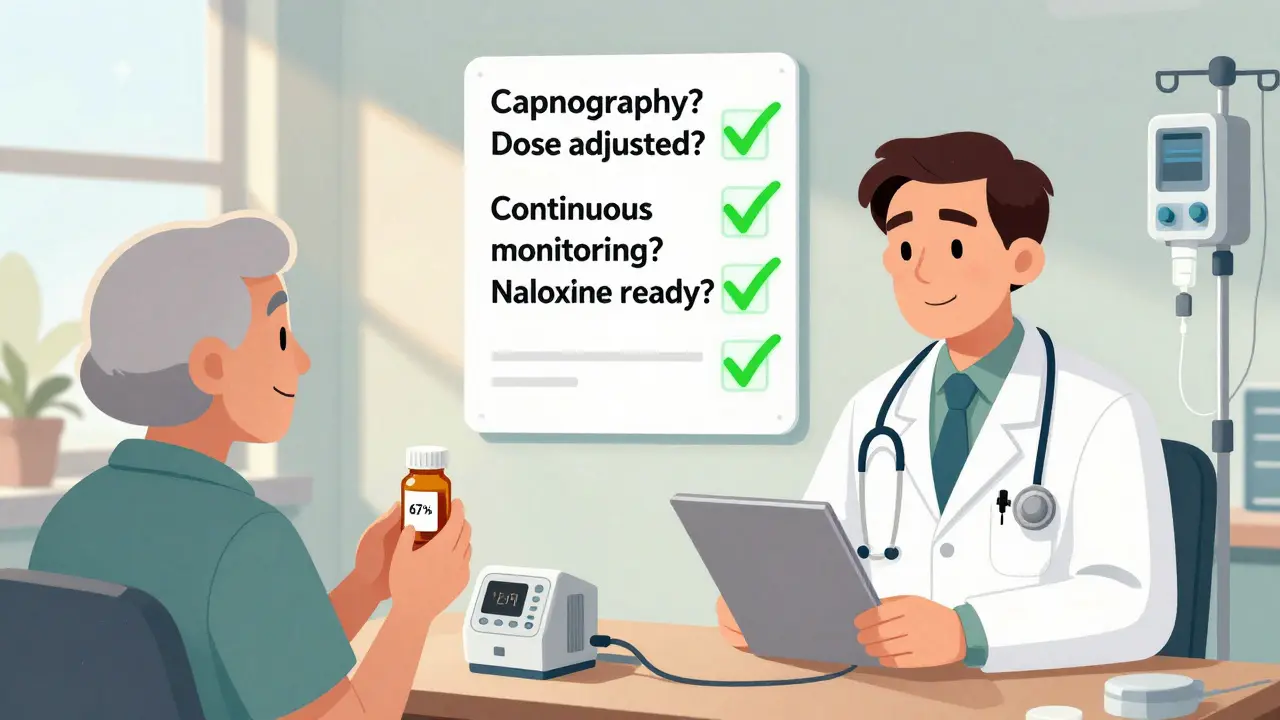
You don’t need a high-tech hospital to protect seniors. Here’s your action plan:- Start with RASS. Train every nurse, aide, and tech to use it. Practice on each other. Get comfortable with the scale.
- Use capnography if you can. Even a basic device makes a difference. If your facility doesn’t have one, push for it. Medicare and Medicaid now tie reimbursement to proper monitoring.
- Adjust doses. Never give the standard adult dose to someone over 60. Use the formula. When in doubt, give less.
- Monitor continuously. No more 5-minute checks. If you’re giving sedation, you need someone watching the patient 24/7. One nurse per patient is the minimum.
- Have naloxone ready. If opioids are involved, keep it on hand. Know how to use it. Don’t wait for someone to stop breathing.
Final Thought: Technology Helps, But People Save Lives
The best monitor in the world won’t help if no one’s paying attention. A 2004 report found that 28% of monitoring failures happened because staff trusted the machine over their own eyes. A pulse oximeter showing 87%? Maybe it’s a bad signal. Maybe the patient’s nails are painted. Maybe they’re not breathing. Don’t assume. Check. Ask. Feel.Saving seniors from overdose isn’t about having the latest gadget. It’s about being present. Watching. Listening. Acting before the alarm sounds.
What are the first signs of opioid overdose in seniors?
The earliest signs are slow breathing (fewer than 8 breaths per minute), unresponsiveness to voice or touch, and a drop in the Richmond Agitation-Sedation Scale (RASS) score to -3 or lower. Skin may feel cool or clammy, and lips or fingertips may turn blue. Unlike younger adults, seniors often don’t show obvious pinpoint pupils or extreme drowsiness-making these signs easy to miss.
Is pulse oximetry enough to monitor seniors on sedatives?
No. Pulse oximetry alone misses up to 40% of dangerous breathing events in seniors, especially those on supplemental oxygen. It shows oxygen levels, but not whether the person is breathing. Capnography, which measures carbon dioxide, detects apnea 12-14 minutes earlier. Always combine it with capnography or another ventilation monitor.
How much should I reduce sedative doses for seniors?
Use this formula: Adjusted dose = standard adult dose × (1 - 0.005 × (age - 20)). For a 75-year-old, that’s about 67% of the standard dose. For someone 85, reduce to about 57%. Always start low and go slow. Even small reductions make a big difference in safety.
Can over-sedation happen outside of hospitals?
Yes. Over 40% of outpatient endoscopy centers still don’t use continuous capnography for seniors, according to the 2022 SGNA survey. Many seniors receive sedatives for dental work, colonoscopies, or minor procedures at clinics or doctor’s offices. Without proper monitoring, these settings are high-risk zones. Always ask: ‘Are you using capnography and continuous monitoring?’
What should I do if I suspect an overdose?
Stop giving any sedatives or opioids immediately. Call for help. Open the airway and give oxygen if available. If opioids are involved, administer naloxone (Narcan) as directed. Start rescue breathing if breathing has stopped. Do not wait for EMS-every minute counts. Record vital signs and the timeline of events for medical teams.
Next Steps for Families and Caregivers
If you’re caring for an elderly loved one who needs sedation-whether for surgery, a procedure, or chronic pain-ask these questions before any treatment:- Will you be using capnography or another breathing monitor?
- Will the sedative dose be adjusted for age?
- Will someone be watching continuously, not just checking every few minutes?
- Do you have naloxone on hand if opioids are used?
If the answer is ‘no’ to any of these, push for better. Your loved one’s life depends on it.


Aayush Khandelwal on 31 December 2025, AT 11:59 AM
Yo, this post is a godsend. Capnography isn't just a gadget-it's the only thing standing between a 78-year-old and a coffin. I've seen nurses ignore it because 'the oximeter looks fine.' Bro, that's like using a GPS that only shows your fuel level and not the road ahead. Silent hypoxia doesn't care if you're busy. It just kills. And don't even get me started on the 'standard dose' myth. That's not medicine, that's Russian roulette with morphine.