Hemochromatosis isn’t a rare curiosity-it’s a silent killer hiding in plain sight. Imagine your body absorbing iron like a sponge, even when it’s already full. Over time, that extra iron doesn’t just sit around. It piles up in your liver, heart, pancreas, and joints, slowly damaging them until you’re left with fatigue, joint pain, diabetes, or even liver cancer. And here’s the twist: most people don’t know they have it until it’s too late. This isn’t about taking too many iron supplements. This is genetic. Your body is wired to absorb too much iron from food, and without treatment, it will destroy you.
What Exactly Is Hemochromatosis?
Hemochromatosis is a genetic disorder that makes your body absorb way more iron than it needs. Normally, your gut takes in just enough iron to replace what you lose through blood loss or skin shedding. But if you have two copies of the mutated HFE gene-especially the C282Y mutation-your body loses the brake that controls iron absorption. Hepcidin, the hormone that tells your intestines to slow down iron uptake, stops working. So your body keeps pulling in iron, even when it’s already overflowing.
This isn’t something that happens overnight. It creeps in over decades. Men usually start showing symptoms between 30 and 50. Women often don’t notice anything until after menopause, because monthly periods naturally flush out excess iron. By then, it’s often too late. About 1 in 200 people of Northern European descent carry two copies of the faulty gene. That’s over a million Americans alone. And only 10 to 15% of them have been diagnosed.
How Do You Know You Have It?
The symptoms are vague. Fatigue. Joint pain. Brain fog. Loss of sex drive. These get blamed on stress, aging, or depression. A 2023 survey of patients found that 68% saw 3 to 5 doctors over 5 to 7 years before getting the right diagnosis. That’s not a failure of the patient-it’s a failure of the system.
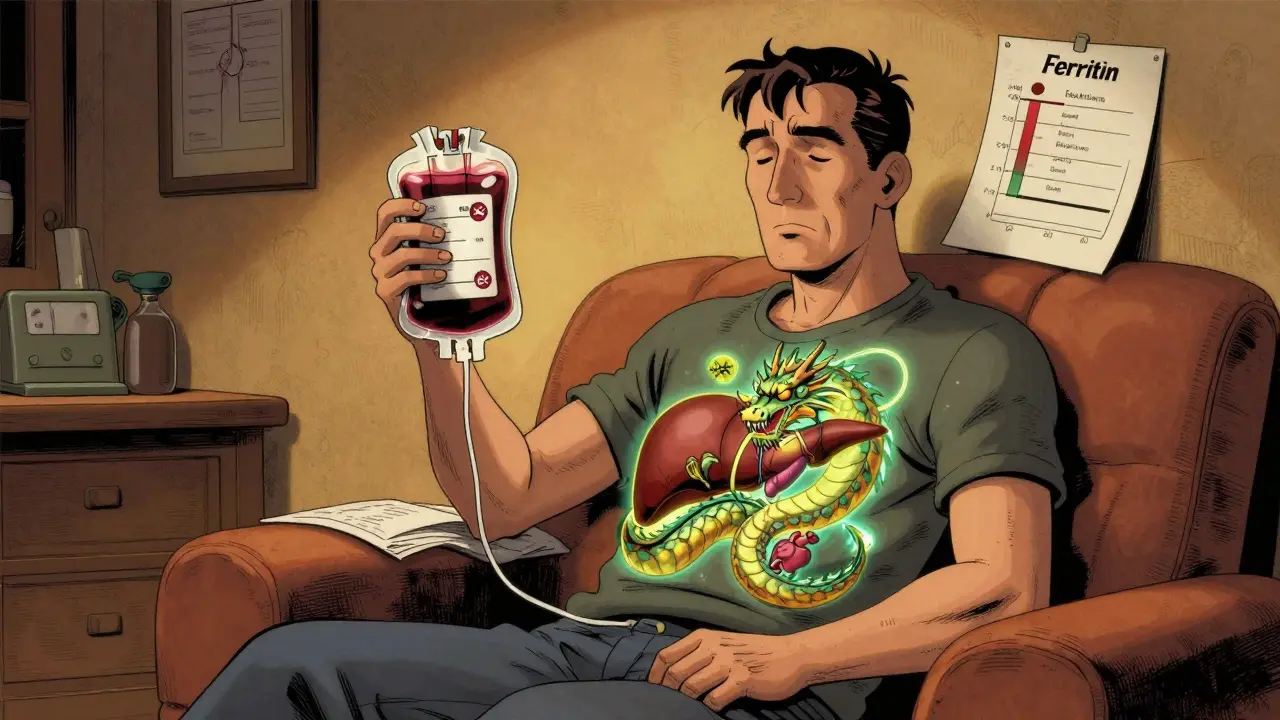
But there are clear lab markers. The first red flag is high transferrin saturation-above 45%. That’s the percentage of iron bound to the protein that carries it in your blood. Normal is under 45%. If it’s higher, your body is absorbing too much iron. The next step is checking serum ferritin. This measures how much stored iron you have. In men, anything over 300 ng/mL is suspicious. In women, over 200 ng/mL. If both are high, and you have the HFE gene mutation, the diagnosis is almost certain.
And here’s the kicker: if your ferritin is above 1,000 ng/mL, you have a 50 to 75% chance of already having liver cirrhosis. That’s not reversible. Once you hit that number, your risk of liver cancer skyrockets. Early detection is the only thing that stops this.
Phlebotomy: The Simple Treatment That Works
The treatment for hemochromatosis is shockingly simple: take blood out. Not a drug. Not a pill. Just a needle and a bag. That’s phlebotomy-the same process used by blood donors.
Each time you donate 500 mL of blood, you lose about 200 to 250 milligrams of iron. Your body can’t absorb new iron fast enough to replace it, so your iron stores drop. It’s like turning off a leaky faucet while draining the tub.
The process has two phases. First, the induction phase: you get a phlebotomy every week until your ferritin hits 50 to 100 ng/mL. For someone with ferritin at 2,500, that might take 30 to 50 sessions over 12 to 18 months. Reddit user u/HemoWarrior needed 62 sessions over 15 months. That’s a lot of needles. But it’s the only thing that stops the damage.
Then comes maintenance. Once your iron is under control, you don’t stop. You keep going-every 2 to 4 months. Most people need 4 to 6 sessions a year to stay in the safe zone. Skipping maintenance is the number one reason people end up with liver disease. Symptoms disappear after a few sessions. That’s when people think they’re cured. They’re not. The gene is still there. The iron will come back.
Why Don’t More People Get Treated?
Many patients report vein access problems as they get older. Some blood centers won’t do therapeutic phlebotomy because they’re set up for donations, not medical care. Others can’t find a doctor who knows how to manage it. A 2023 survey by the American Hemochromatosis Society found that 42% of patients quit maintenance therapy after a couple of years-not because they felt better, but because no one reminded them it was lifelong.
And cost? It’s almost nothing. Each phlebotomy costs $0 to $50 if covered by insurance. Compare that to iron chelation drugs like deferasirox, which run $25,000 to $35,000 a year. Chelators are reserved for people who can’t tolerate blood removal-like those with severe anemia or heart damage from iron overload. For 95% of patients, phlebotomy is the gold standard.
What Happens If You Don’t Treat It?
Left untreated, hemochromatosis follows a predictable path. First, fatigue and joint pain. Then, skin turns bronze or gray-not from sun exposure, but from iron deposits. Next, diabetes develops because iron destroys insulin-producing cells in the pancreas. After that, the liver starts to scar. Cirrhosis sets in. Then, liver cancer. Heart rhythm problems follow. Testosterone crashes. Men lose libido. Women lose periods.
Survival rates tell the story. If you’re diagnosed before ferritin hits 1,000 ng/mL, your 10-year survival rate is 95%. If you’re diagnosed after cirrhosis develops? That drops to 60%. That’s not a small difference. That’s life or death.
Who Should Get Tested?
You don’t need to wait for symptoms. If you have a family member with hemochromatosis, get tested. Cascade screening-testing relatives after one person is diagnosed-finds 70% of new cases. That’s the most effective public health strategy we have for this disease.
Also, if you have unexplained liver enzyme elevations, diabetes, cardiomyopathy, or chronic fatigue, ask your doctor for a transferrin saturation and serum ferritin test. Most primary care doctors don’t order these routinely. Only 12% check transferrin saturation for patients with fatigue or joint pain, according to the American Association for Clinical Chemistry. But those two tests cost less than $50 and can save your life.
The Future of Treatment
There’s promising research on the horizon. A new drug called PTG-300 mimics hepcidin-the hormone your body stops making. In Phase 2 trials, it reduced transferrin saturation by 53% in 12 weeks. That could mean fewer phlebotomies in the future. But it’s still experimental. For now, blood removal is the only proven, safe, and affordable treatment.
Also, genetic testing is cheaper than ever. In 2023, a full HFE gene test costs $150 to $300. That’s a fraction of what it cost in 2000. If you’re of Northern European descent and have a family history, getting tested is a no-brainer.
What You Can Do Today
Don’t wait for symptoms. If you have a parent, sibling, or child with hemochromatosis, get your transferrin saturation and ferritin tested. If you’re over 30 and have unexplained fatigue, joint pain, or low libido, ask for those tests. If your numbers are high, get genetic testing. If you’re diagnosed, start phlebotomy immediately. Don’t stop when you feel better. Keep going. Maintenance is non-negotiable.
Hemochromatosis isn’t a death sentence. It’s a treatable condition-if you catch it early. The tools are simple. The treatment is cheap. The stakes couldn’t be higher. Your liver doesn’t ask for permission before it fails. Neither should you.
Can hemochromatosis be cured?
No, hemochromatosis cannot be cured because it’s a genetic condition. But it can be completely managed. With regular phlebotomy to keep iron levels low, people with hemochromatosis can live normal, healthy lives without liver damage, diabetes, or heart problems. The key is lifelong maintenance treatment-even after symptoms disappear.
Is phlebotomy safe?
Yes, phlebotomy is very safe when done under medical supervision. Each session removes about 500 mL of blood, similar to a blood donation. Side effects are rare and usually mild-like dizziness or fatigue afterward. Serious complications are extremely uncommon. It’s far safer than long-term drug treatments or invasive procedures. Most patients tolerate it well, even after dozens of sessions.
Can you get hemochromatosis from eating too much iron?
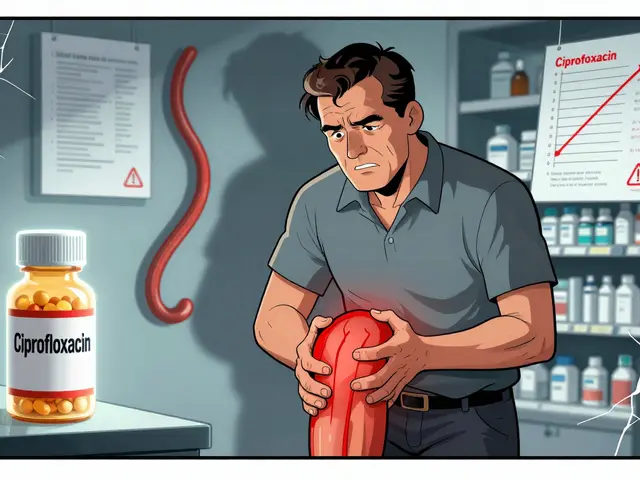
No. Hemochromatosis is genetic. Eating iron-rich foods or taking supplements won’t cause it. But if you already have the gene mutation, eating excess iron or taking iron supplements can speed up damage. People with hemochromatosis are advised to avoid iron supplements, vitamin C with meals (which boosts iron absorption), and raw shellfish (risk of infection when iron is high).
How often do you need phlebotomy after diagnosis?
It depends on your iron levels. Initially, you’ll need weekly sessions until ferritin drops to 50-100 ng/mL, which can take over a year. After that, maintenance is usually every 2 to 4 months. Most people need 4 to 6 sessions per year. Your doctor will adjust the schedule based on your ferritin and hemoglobin levels.
Can women with hemochromatosis have children?
Yes, but only if iron levels are controlled. High iron can affect fertility and increase risks during pregnancy. Women with hemochromatosis should aim for ferritin below 100 ng/mL before trying to conceive. During pregnancy, phlebotomy is usually paused, and iron levels are monitored closely. With proper management, most women have healthy pregnancies.
Does alcohol make hemochromatosis worse?
Absolutely. Alcohol increases iron absorption and directly damages the liver. For someone with hemochromatosis, drinking alcohol multiplies the risk of cirrhosis and liver cancer. Doctors strongly recommend complete abstinence. Even moderate drinking can push someone with early-stage disease into advanced liver damage.
Is genetic testing necessary if ferritin is high?
Yes. High ferritin can come from many causes-alcohol, obesity, hepatitis, or chronic inflammation. Only genetic testing for HFE mutations (C282Y, H63D) confirms hereditary hemochromatosis. Without it, you can’t rule out other conditions or know if your family members are at risk. Genetic testing is the only way to confirm the diagnosis and guide family screening.

James Dwyer on 27 January 2026, AT 17:50 PM
Hemochromatosis is one of those conditions that should be screened for during routine blood work, especially if you're of Northern European descent. I had no idea I had it until my ferritin hit 1,200. Now I get phlebotomy every 3 months like clockwork. No symptoms, no complications. It’s not rocket science-it’s just consistent care.
People think it’s rare, but it’s not. It’s just invisible until it’s too late.