Managing diabetes isn’t just about checking blood sugar levels-it’s about understanding the medicines you’re taking and what they might do to your body. With so many options available, from old-school pills to newer injectables, it’s easy to feel overwhelmed. You’re not alone if you’ve wondered: What side effects should I expect? And more importantly, how do I know if what I’m feeling is normal-or something I need to act on?
Metformin: The First-Line Choice with Common, Manageable Side Effects
Most people with type 2 diabetes start with metformin. It’s cheap, effective, and has been used for decades. But about 1 in 3 people experience stomach trouble when they begin taking it. Nausea, diarrhea, bloating-these aren’t rare. A 2021 study in JAMA Internal Medicine found 26% of users had nausea, 23% had diarrhea. It’s not dangerous, but it’s uncomfortable enough that nearly half of people quit within the first month.
The fix? Start low. Take 500 mg once a day with dinner, not on an empty stomach. After a week or two, your body adjusts. Many switch to the extended-release version, which cuts GI side effects by about half. If you’re still struggling after a month, talk to your doctor-there are other options.
There’s another hidden issue: long-term metformin use can lower your vitamin B12 levels. The NHS recommends annual blood tests if you’ve been on it for five years or more. Low B12 causes fatigue, tingling in hands and feet, even memory problems. It’s easily fixed with supplements-usually a monthly injection or daily oral dose. Don’t ignore it. Left untreated, nerve damage can become permanent.
Sulfonylureas: Effective but Risky for Low Blood Sugar
Drugs like glyburide and glipizide force your pancreas to make more insulin. They work quickly and are inexpensive. But they come with a big catch: hypoglycemia. About 1 in 6 people on these pills have at least one low blood sugar episode every year. And if you skip a meal, drink alcohol, or exercise more than usual? The risk jumps.
Low blood sugar isn’t just dizziness or shakiness. It can lead to confusion, seizures, or even loss of consciousness. That’s why so many people who’ve had a bad episode switch away from these drugs. A 2022 survey found that 78% of patients who experienced hypoglycemia with sulfonylureas preferred newer, safer options-even if they cost more.
Also, these pills cause weight gain. On average, people gain 2 to 4 kg in the first year. For someone already struggling with insulin resistance, that’s a setback. If you’re trying to lose weight or have heart issues, this isn’t the best fit.
Thiazolidinediones: Weight Gain and Heart Risks
Pioglitazone (Actos) makes your body respond better to insulin. It’s useful if you’re insulin resistant, especially with fatty liver or polycystic ovary syndrome. But it comes with trade-offs. About 1 in 20 people develop fluid retention-swollen ankles, sudden weight gain. That’s a red flag for heart failure, especially if you already have heart problems.
The PROactive trial back in 2005 showed a 43% higher risk of heart failure with pioglitazone. It’s not a deal-breaker for everyone, but doctors now avoid it in people with existing heart disease. Weight gain is another downside-2 to 3 kg on average. And while it doesn’t cause low blood sugar on its own, combining it with insulin or sulfonylureas increases that risk.
It’s also been linked to a small increase in bladder cancer risk, though the evidence isn’t conclusive. If you’ve had bladder cancer or blood in your urine, avoid this class entirely.
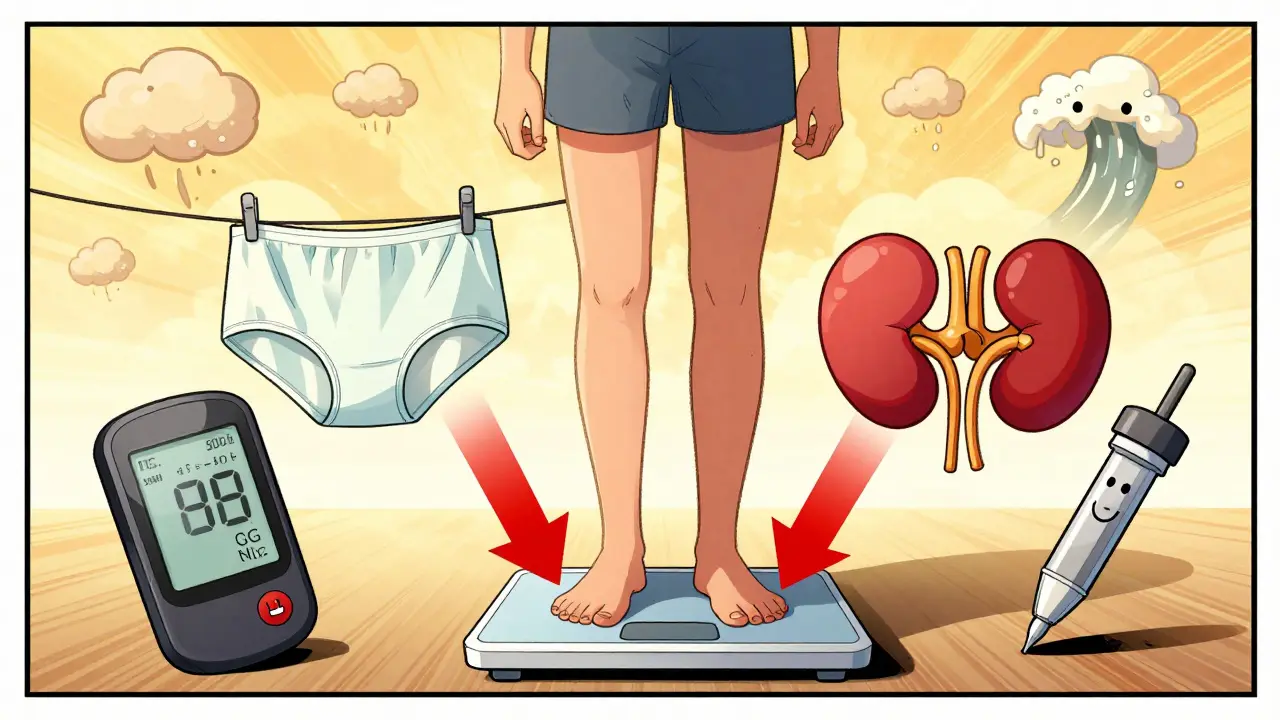
SGLT2 Inhibitors: Weight Loss and Infections
Drugs like empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana) work by making your kidneys flush out extra sugar through urine. The result? Lower blood sugar, weight loss, and better heart and kidney protection.
But here’s what most people don’t expect: genital yeast infections. In women, it’s about 1 in 7. In men, it’s 1 in 20. It’s not serious, but it’s annoying-itching, redness, discomfort. The fix? Keep the area clean and dry. Wear cotton underwear. Avoid douches or scented products. A 2022 study from UCSF showed this simple change cuts recurrence by 60%.
Another rare but dangerous risk: diabetic ketoacidosis (DKA). It happens in less than 1 in 300 users, but it’s serious. Symptoms: nausea, vomiting, stomach pain, confusion, fruity-smelling breath. If you’re sick, not eating, or cutting carbs drastically, your risk goes up. Always check ketones if you feel off-even if your blood sugar isn’t high.
Also, dehydration is common. You’re peeing out sugar and water. Drink more fluids, especially in hot weather or when exercising. If you feel lightheaded, dizzy, or have dry mouth, check with your doctor.
GLP-1 Receptor Agonists: Powerful but Tough on the Stomach
Liraglutide (Victoza), semaglutide (Ozempic, Wegovy), and dulaglutide (Trulicity) are injectables that mimic a natural hormone. They slow digestion, reduce appetite, and help your body make insulin only when needed. They’re among the most effective drugs for weight loss and heart protection.
But the side effects? They’re real. Up to half of users feel nauseous. One in five vomit. Diarrhea is common too. Most people get used to it within weeks. Start with the lowest dose. Don’t rush the increase. Eat smaller meals. Avoid greasy or spicy foods. If nausea lasts longer than a month, talk to your doctor-it might not be worth it for you.
There’s also a small risk of pancreatitis (inflammation of the pancreas). Symptoms: severe, constant belly pain that radiates to your back. If this happens, stop the drug and get help immediately.
On the upside, most people lose 5 to 10 kg in six months. Blood sugar drops. Blood pressure improves. Heart attacks and strokes go down by up to 26%. For many, the trade-off is worth it.
Insulin: The Most Effective, But With the Highest Risk
Insulin is the only option for type 1 diabetes. Many with type 2 eventually need it too. It’s powerful. But it’s also the most dangerous if misused.
Low blood sugar is the biggest concern. People on intensive insulin therapy have 15 to 30 episodes per year. Some are mild-shakiness, sweating. Others are severe-passing out, needing glucagon injections. Fear of lows causes many to under-dose, which means higher blood sugar over time. That’s a dangerous cycle.
Weight gain is common too-2 to 5 kg on average. That’s because insulin helps your body store fat. It’s not your fault. It’s biology.
Continuous glucose monitors (CGMs) have changed everything. They alert you before your sugar drops too low. The DIAMOND trial showed CGMs reduce severe lows by 40%. If you’re on insulin and not using one, ask your doctor. It’s not optional anymore-it’s essential.
Injection site reactions-redness, lumps-are rare but can happen if you don’t rotate sites. Always change where you inject. Use a new needle every time. Don’t reuse.
Tirzepatide: The New Kid on the Block
Approved in 2022, tirzepatide (Mounjaro) is a dual-action drug that works like GLP-1 and GIP. It’s the most effective weight-loss drug for diabetes so far. In trials, people lost 15 to 20% of their body weight. That’s more than any other diabetes drug.
And here’s the surprise: it causes less nausea than semaglutide. Only 24% of users had nausea, compared to 35% with Ozempic. That makes it easier to stick with.
It’s expensive-over $900 a month without insurance. But if you’re struggling with weight, heart disease, or kidney problems, it might be worth the cost. The FDA approved it for type 2 diabetes only, but doctors are increasingly prescribing it off-label for obesity, even without diabetes.
What to Do When Side Effects Hit
Side effects don’t mean you should quit. They mean you need to adjust.
- For GI issues: Start low, go slow. Use extended-release forms. Eat smaller meals.
- For low blood sugar: Learn the 15-15 rule. Keep glucose tablets handy. Use a CGM.
- For infections: Hygiene matters. Cotton underwear, no douches, dry skin.
- For weight gain: Combine meds with movement. Even 20 minutes of walking daily helps.
- For cost: Ask about generics. Metformin costs $4 a month. Ask your pharmacist about patient assistance programs.
Never stop a diabetes drug cold turkey. That can spike your blood sugar dangerously. Always talk to your doctor first.
When to Switch Medications
There’s no one-size-fits-all. But here are clear signs it’s time to reconsider:
- You’ve had two or more severe low blood sugar episodes in six months.
- You’ve had recurring yeast infections for more than three months.
- Your weight is going up, not down-and you’re trying to lose.
- Your blood sugar is still above 8% after three months on the current drug.
- You can’t afford it and it’s causing stress.
Newer drugs like SGLT2 inhibitors and GLP-1 agonists aren’t just better-they’re proven to save lives. They reduce heart attacks, strokes, kidney failure, and death. If you have heart disease, kidney disease, or obesity, these are now the first choices-not metformin alone.
Cost is a barrier. But many drugmakers offer coupons. Some pharmacies have $4 generic programs. Talk to your pharmacist. You’d be surprised what’s available.
What’s Next in Diabetes Treatment
Oral GLP-1 pills are coming. Orforglipron, tested in 2024, caused 10.5% weight loss in early trials-without injections. Once-weekly insulins like icodec are now approved in Europe. Closed-loop systems (artificial pancreases) are getting smarter, adjusting insulin automatically based on real-time glucose data.
But the biggest change isn’t technology. It’s mindset. Diabetes care is no longer just about lowering numbers. It’s about quality of life. Can you sleep without fear of lows? Can you eat without guilt? Can you afford your meds?
That’s the real goal. Not HbA1c under 7%. But living well with diabetes.
Can diabetes medications cause weight loss?
Yes, some do. GLP-1 receptor agonists like semaglutide and tirzepatide cause significant weight loss-often 5 to 20% of body weight. SGLT2 inhibitors like Jardiance and Farxiga lead to modest loss, around 2 to 5 kg, because they flush out sugar and water. Metformin may cause a small loss of 1 to 3 kg. But sulfonylureas and insulin usually cause weight gain.
Is metformin safe for long-term use?
Yes, for most people. It’s been used safely for over 60 years. The main risks are vitamin B12 deficiency after five or more years and mild stomach upset. Both are manageable. Get your B12 checked yearly. Take the extended-release version if GI issues persist. Avoid it if your kidney function drops below 30 mL/min.
Why do SGLT2 inhibitors cause yeast infections?
They work by making your kidneys remove sugar through urine. That sugar ends up in your genital area, creating a perfect environment for yeast to grow. It’s not an infection you catch-it’s one your body creates because of the drug. Keeping the area clean, dry, and wearing cotton underwear reduces the risk by 60%.
Can I stop my diabetes medication if I lose weight?
Sometimes, yes-but never without your doctor’s guidance. Some people with type 2 diabetes who lose 10% or more of their body weight can reduce or even stop meds, especially if they maintain the weight. Blood sugar may stay normal. But this doesn’t mean diabetes is cured. It’s in remission. Stopping meds without monitoring can lead to dangerous spikes. Always test your blood sugar and work with your care team.
Are newer diabetes drugs worth the cost?
If you have heart disease, kidney disease, or obesity, yes. SGLT2 inhibitors and GLP-1 agonists reduce the risk of heart attack, stroke, kidney failure, and death by up to 38%. That’s not just better control-it’s life-saving. If cost is an issue, ask about patient assistance programs. Many drugmakers offer free or discounted meds for qualifying patients. Generic metformin is still the best starter, but newer drugs are the future for high-risk patients.
What should I do if I experience ketoacidosis symptoms?
Ketoacidosis is rare but dangerous. Symptoms include nausea, vomiting, stomach pain, confusion, and fruity-smelling breath. If you’re on an SGLT2 inhibitor and feel this way-even if your blood sugar isn’t high-check your urine or blood for ketones. If ketones are moderate or high, go to the ER immediately. Don’t wait. This can become life-threatening within hours.
Do diabetes medications affect kidney function?
Metformin is avoided if your kidney function is below 30 mL/min. SGLT2 inhibitors actually protect the kidneys-they slow decline in people with chronic kidney disease. GLP-1 agonists also reduce kidney damage over time. Insulin and sulfonylureas don’t harm kidneys directly, but uncontrolled high blood sugar does. The goal is to use meds that protect your kidneys, not just lower sugar.
Final Thoughts: Your Medication, Your Life
Diabetes meds aren’t one-size-fits-all. What works for your neighbor might not work for you. Side effects aren’t failures-they’re signals. They tell you what your body needs. Maybe you need a different drug. Maybe you need a lower dose. Maybe you need better support.
The best treatment isn’t the cheapest. It’s the one you can live with. The one that lets you sleep through the night. The one that doesn’t make you afraid to eat. The one that helps you live longer, not just live with numbers.
Ask questions. Track your symptoms. Talk to your pharmacist. Use your CGM. You’re not just managing diabetes-you’re reclaiming your life.



Paul Huppert on 1 January 2026, AT 19:03 PM
Metformin gave me nausea for weeks, but I stuck with it and switched to XR. Now I barely notice it. Also got my B12 checked last year-low as hell. Took a supplement and my brain fog lifted. Small wins.
Thanks for the clear breakdown.