Statin Discontinuation Risk Calculator
Statin Discontinuation Risk Calculator
This tool helps you understand your risk of heart events after stopping statins based on your health profile. Remember: This is not medical advice. Always talk to your doctor before stopping any medication.
Your Health Profile
More than 39 million Americans take statins every day. These drugs have saved countless lives by lowering cholesterol and preventing heart attacks and strokes. But for many people, especially older adults or those with serious health conditions, the benefits no longer outweigh the downsides. The question isn’t just whether to stop statins-it’s when and how to do it without putting yourself at risk.
Why People Stop Statins
Most people start statins because their doctor told them to. But stopping? That’s usually personal. A 2013 study found nearly one in five patients quit statins for at least a year. And the biggest reason? Side effects. Muscle pain is the number one complaint. It’s not always clear if it’s the statin or just aging, but when a 72-year-old says their legs ache every morning and they can’t climb stairs like they used to, they’re going to wonder: Is this worth it? Fear plays a big role too. Online forums are full of people worried about diabetes, liver damage, or memory loss. Some of these fears are real, others are exaggerated. But the fear alone is enough to make someone quit. And once they stop, many never go back-even if their doctor recommends it.Who Should Consider Stopping
Not everyone should stop. But for some, continuing statins might be doing more harm than good. Older adults with limited life expectancy-say, someone with advanced cancer or severe heart failure-often don’t benefit from long-term statin use. A 2023 clinical guide from MyPCnow says if you have less than two years to live, stopping statins is safe and often the right choice. Why? Because statins take years to show benefit. If you’re not going to live long enough to see that benefit, the daily pill, the side effects, and the cost aren’t worth it. People with multiple chronic conditions are another group. Imagine a 78-year-old with kidney disease, diabetes, and arthritis. They’re already taking eight or nine medications. Adding another daily pill just to lower cholesterol by 20 points? That’s polypharmacy overload. The American Geriatrics Society says in cases like this, deprescribing statins is a smart move. Those who had side effects-even mild ones-should talk to their doctor before continuing. Muscle pain, fatigue, or liver enzyme changes aren’t reasons to panic, but they are reasons to pause and reassess.What Happens When You Stop
Stopping statins doesn’t mean your cholesterol instantly spikes back to dangerous levels. But it does mean your risk of heart events starts creeping up again. A 2021 study in JAMA Network Open tracked over 100,000 people who stopped statins. The results were clear:- For people with existing heart disease (secondary prevention), stopping led to one extra major heart event for every 77 people who quit per year.
- For people without heart disease (primary prevention), the risk was lower: one extra event for every 112 people who stopped.
How to Stop Safely
Never just quit cold turkey. Even if you’re done with statins, you need a plan. Step 1: Talk to your doctor. Don’t make this decision alone. Bring up your concerns. Say: “I’m tired of the side effects. Is this still right for me?” A good doctor will listen, not push back. Step 2: Review your risk. Are you in secondary or primary prevention? Do you have diabetes? High blood pressure? A family history of early heart disease? Your risk level determines how dangerous stopping is. Step 3: Consider alternatives. If muscle pain is the issue, switching to a different statin at a lower dose might help. Rosuvastatin and pravastatin are less likely to cause muscle problems. Or try intermittent dosing-taking the pill every other day or twice a week. Some studies show this still lowers cholesterol enough without the side effects. Step 4: Try non-statin options. For some, ezetimibe (a cholesterol absorption blocker) or PCSK9 inhibitors (injections) might work. But they’re expensive. Fibrates and omega-3s help too, but they’re not as powerful. Don’t switch just because you’re scared of statins-switch because it’s a better fit. Step 5: Monitor after stopping. Get your cholesterol checked 4 to 6 weeks after quitting. If it jumps back to dangerous levels, you might need to reconsider. Also watch for symptoms: chest pain, shortness of breath, dizziness. Call your doctor if they come back.What Your Doctor Should Do
Doctors aren’t always ready to talk about stopping statins. Too often, they assume “once prescribed, always prescribed.” But that’s outdated thinking. A 2020 review in the Journal of the American Geriatrics Society found that three major guidelines now suggest considering statin discontinuation in patients with poor health. That’s progress. Doctors should:- Ask older patients every year: “Are you still comfortable taking this?”
- Document the reason for stopping-not just “no longer necessary,” but “muscle pain,” “limited life expectancy,” or “patient preference.”
- Involve pharmacists. They’re trained in deprescribing and can help sort out what’s needed and what’s not.
- Use tools like the ASCVD Risk Calculator to re-evaluate benefit over time.
What’s Coming Next
A major clinical trial called “Discontinuing Statins in Multimorbid Older Adults” is underway in Europe. It’s tracking 1,800 people over 65 with multiple health issues. Half will stop statins. Half will keep taking them. The goal? To see if stopping affects quality of life, muscle strength, falls, and heart events over two years. If the results show no harm from stopping, this could change how doctors treat older patients everywhere. Meanwhile, companies are developing genetic tests to predict who’s likely to have side effects. Imagine a blood test that tells you: “You’re 80% more likely to get muscle pain on simvastatin.” That could make statin use way more personalized.Final Thoughts
Statins are powerful. But they’re not magic. They’re tools. And like any tool, they’re only useful if they fit the job. If you’re young, healthy, and have a family history of heart disease? Keep taking them. The data is clear: they save lives. If you’re older, frail, or have a short life expectancy? Stopping might be the right move. The goal isn’t to live longer-it’s to live better. And sometimes, that means fewer pills, less pain, and more peace. The truth? No one should take a pill for life without rethinking it. Statins are no exception. Your health isn’t a one-size-fits-all prescription. It’s a conversation. And you deserve to be part of it.Can I stop statins on my own?
No. Stopping statins without medical guidance can raise your risk of heart attack or stroke, especially if you have existing heart disease. Always talk to your doctor first. They can help you decide if stopping is safe and how to do it properly.
Do statins cause muscle pain in everyone?
No. Most people-over 90%-don’t have muscle pain from statins. But for the small number who do, it can be real and disabling. The pain is often in the shoulders, thighs, or calves and gets worse with activity. If you suspect it’s the statin, don’t assume it’s just aging. Tell your doctor. There are ways to manage it, including switching statins or lowering the dose.
Is it safe to stop statins if I’m over 75?
It depends. If you’re healthy and have no history of heart disease, stopping might be safe. If you’ve had a heart attack, stroke, or stent, stopping increases your risk. The American Geriatrics Society says older adults with poor health, limited life expectancy, or multiple medications should consider stopping. But it’s not automatic-it’s a personal decision based on your health goals.
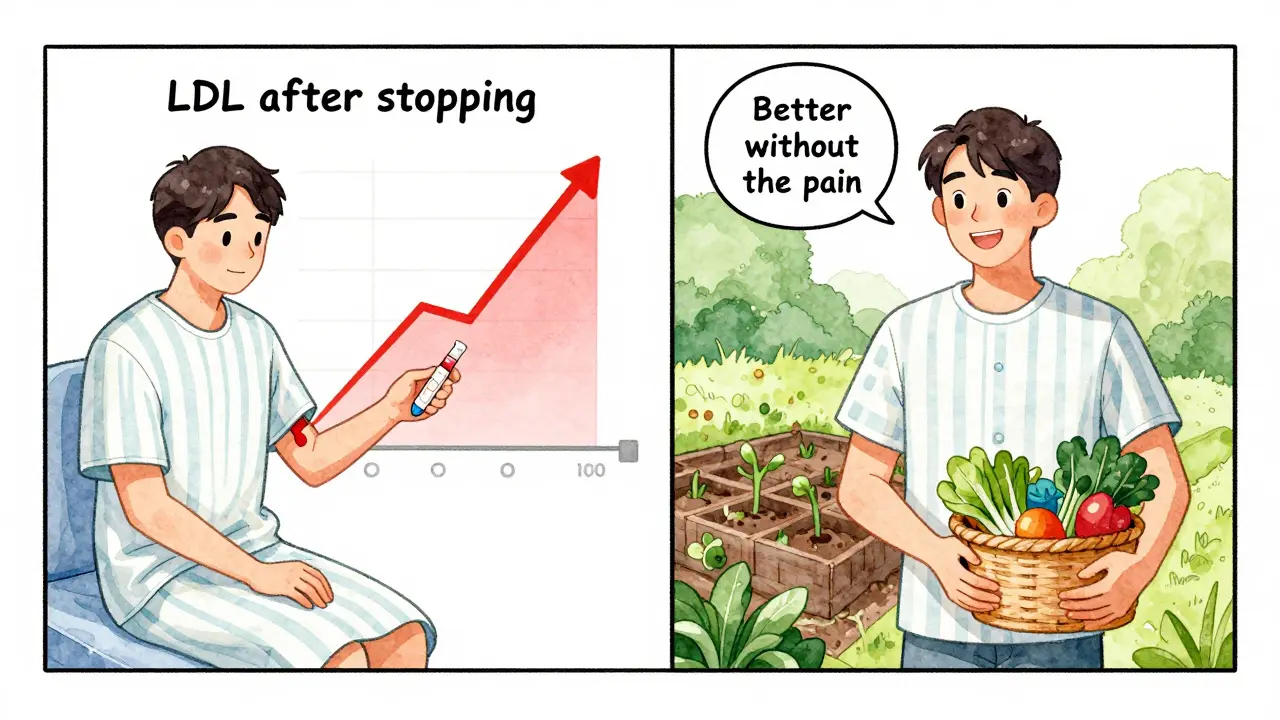
What happens to my cholesterol if I stop statins?
Your LDL (bad) cholesterol will likely rise again within weeks. But how high it goes depends on your genetics, diet, and overall health. If you were taking statins for primary prevention, your cholesterol might return to near pre-treatment levels. If you have heart disease, the rise could be faster and more dangerous. That’s why doctors recommend checking your levels 4 to 6 weeks after stopping.
Are there natural ways to lower cholesterol after stopping statins?
Yes, but they’re not as powerful. Eating more fiber (oats, beans, vegetables), reducing saturated fat, exercising regularly, and losing weight can help lower cholesterol by 10-20%. Some supplements like plant sterols or red yeast rice may help too-but they’re not regulated like medications. If your risk is high, lifestyle changes alone usually aren’t enough. Talk to your doctor about whether you still need medication.
Can I restart statins later if I change my mind?
Yes. Many people stop statins and later restart, especially if they develop new heart problems or their risk increases. But restarting isn’t always easy. Some people have worse side effects the second time around. If you plan to restart, do it under medical supervision. Your doctor might choose a different statin or a lower dose.
Does stopping statins improve quality of life?
For some, yes. People who stop because of muscle pain, fatigue, or sleep problems often report feeling better within weeks. A 2024 study found that older adults who discontinued statins had improved physical function and fewer falls. But this isn’t true for everyone. If your main concern is preventing a heart attack, stopping might not improve your quality of life-it could threaten it. The key is matching your decision to your personal health goals.


Lyle Whyatt on 8 February 2026, AT 07:26 AM
Look, I get it - statins are a godsend for some, but for others? They’re just another pill in a pile that makes you feel like a walking pharmacy. My dad, 79, had a stent in 2018, but he’s got COPD, kidney issues, and takes 11 meds. He stopped simvastatin last year after his muscle pain got so bad he couldn’t hold his coffee cup. We were terrified, but his doc ran the numbers - his 10-year ASCVD risk dropped from 22% to 18% after he quit. He’s got more energy, sleeps better, and hasn’t had a cardiac event since. Sometimes, the goal isn’t longevity - it’s dignity. And yeah, his cholesterol went up 30 points. But he’s walking his dog every morning, and that’s worth more than a number on a lab report.