When you take a new medication, the side effects listed on the label don’t tell the whole story. That’s because those side effects come from clinical trial data-a tightly controlled snapshot of what happened in a small group of people under ideal conditions. But what happens when millions of real people start taking that same drug? That’s where real-world side effects come in. And they often tell a very different story.
Why Clinical Trials Don’t Show the Full Picture
Clinical trials are designed to answer one question: Does this drug work? Safety is important, but it’s secondary. Participants are carefully selected-you must be healthy enough to join, not taking other risky meds, and usually between 18 and 65. People with multiple chronic conditions? Excluded. Pregnant women? Excluded. Older adults with kidney problems? Often left out. In fact, the median phase 3 cancer trial includes just 381 people. That’s not enough to catch side effects that happen in 1 in 1,000 or 1 in 10,000 people.They also monitor side effects in a very specific way. You show up for checkups every week or month. If you feel dizzy or nauseous, you report it then. But what if your fatigue hits at 10 p.m. after you’ve already left the clinic? Or if your joint pain only shows up after six months of use? Those get missed. The system uses a standardized list called CTCAE v5.0, which has 790 exact terms for grading side effects from mild to fatal. But in real life, people don’t use those terms. They say, “I just can’t get out of bed,” or “My brain feels foggy.”
What Real-World Data Actually Shows
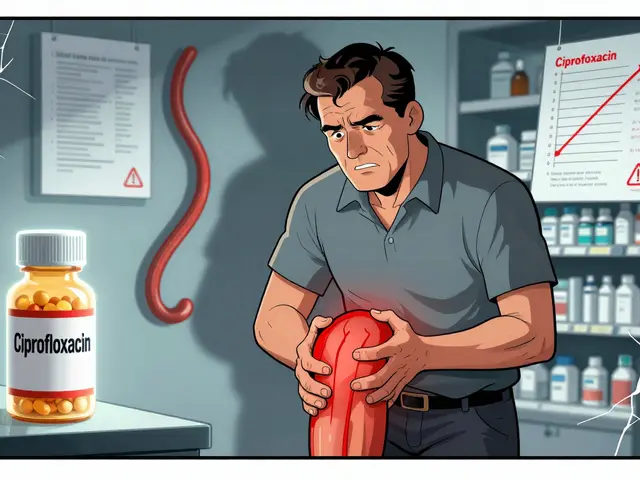
Real-world data comes from the messy, uncontrolled world where drugs are actually used. That means millions of people-different ages, different health conditions, different lifestyles-all taking the same medicine. This data flows into systems like the FDA’s FAERS, which got over 2.1 million adverse event reports in 2022. Hospitals, pharmacies, insurance claims, and even apps like MyTherapy (used by 1.2 million people) are feeding in information.Here’s the kicker: real-world data catches things clinical trials never saw. Take rosiglitazone, a diabetes drug approved in 1999. The trials said it was safe. But after millions of people started taking it, real-world studies found a 43% higher risk of heart attacks. That’s not a small number. It’s life-or-death. And it wasn’t found until years later, when researchers looked at 42,710 patients using the drug versus nearly 160,000 using a similar one.
Another example: pioglitazone. Clinical trials didn’t flag heart failure as a major risk. But real-world data-tracking over 190,000 patients over 10 years-did. The FDA issued a safety warning in 2020 because of that evidence.
The Dark Side of Real-World Data
Real-world data isn’t perfect. In fact, it’s full of noise. People report side effects for all kinds of reasons. Maybe they had the flu. Maybe their stress spiked. Maybe they started a new supplement. That’s why real-world studies sometimes find false alarms.In 2018, a big real-world study claimed anticholinergic drugs (used for allergies, depression, and overactive bladder) caused dementia. It made headlines. But later, deeper analysis showed the real culprit was the underlying conditions-like depression or urinary problems-that led people to take those drugs in the first place. The drugs weren’t causing dementia; the diseases were.
And then there’s underreporting. Only 2 to 5% of actual side effects ever make it into official databases like FAERS. Why? Because doctors are busy. A 2021 AMA survey found only 12% of physicians report side effects regularly. It takes 22 minutes per report. Most just don’t have the time.
Patients Are Seeing What Trials Miss
Patients aren’t waiting for official reports. They’re tracking their own symptoms. On Reddit’s r/Pharmacy, pharmacists say 78% of the time, the side effects they see in real life don’t match what’s listed in clinical trial data. Especially with newer drugs like GLP-1 agonists (think Ozempic, Wegovy). People report nausea, fatigue, brain fog, and hair loss far more often than trials suggested.A 2022 survey by the National Patient Advocate Foundation found that 63% of patients experienced side effects not listed on their FDA-approved labels. Over 40% of those were moderate to severe-enough to mess up their jobs, relationships, or daily routines. One patient wrote: “The trial asked if I was tired during my appointment. But I was fine then. I was exhausted every night after dinner. No one ever asked about that.”
How the FDA Is Catching Up
The FDA knows clinical trials aren’t enough. Since the 21st Century Cures Act in 2016, they’ve been building systems to use real-world data. By 2022, 67% of new drug approvals included real-world evidence in their post-marketing safety plans. That’s up from just 29% in 2017.The Sentinel Initiative, launched in 2008, now monitors 300 million patient records in near real-time. It uses 17 different statistical methods to spot unusual patterns. For example, if a drug suddenly shows a spike in liver damage reports across multiple hospitals, Sentinel flags it. That’s how they caught early signals about ivermectin side effects during the pandemic-47 days before formal reports came in.
But here’s the gap: the EU still requires clinical trials to confirm every new safety signal. The FDA is more flexible. That’s why U.S. patients often get new warnings faster. And now, companies like Pfizer and Johnson & Johnson are building real-world data collection right into late-stage clinical trials. Hybrid studies are becoming the norm.
What This Means for You
If you’re taking a new medication, don’t assume the label tells you everything. Side effects that seem rare in trials might be common in real life. If you notice something unusual-fatigue, mood changes, dizziness, skin rashes, trouble sleeping-track it. Write down when it happens, how bad it is, and what else you’re taking. Talk to your pharmacist. They see more real-world patterns than most doctors.And if you’re on a drug that’s been out for more than a few years, check the FDA’s website for updated safety communications. The warnings you see now might not have existed when you started taking it.
Real-world data won’t replace clinical trials. But it’s the missing piece. Trials tell you if a drug works. Real-world data tells you how it affects real people-over time, in messy lives, with other conditions, and under daily stress. Together, they give you the full picture.
Why are side effects in real life different from what’s listed in clinical trials?
Clinical trials use small, carefully selected groups under strict conditions. Real-world use includes millions of people with different ages, health conditions, and lifestyles. Side effects that are rare in trials-like fatigue after dinner or brain fog-often show up more often in daily life because they’re not captured during scheduled clinic visits.
Can real-world data be trusted if it’s so messy?
Yes, but it needs careful analysis. Real-world data has noise-false signals from unrelated health issues. That’s why agencies like the FDA use advanced statistical tools to filter out coincidences. When multiple sources (EHRs, claims data, patient apps) show the same pattern, it’s more likely to be real. The key is not to trust one study, but to look for consistent signals across many systems.
How long does it take for a real-world side effect to be officially recognized?
It can take months to years. A signal might appear in social media or patient apps within weeks of a drug launch. But formal FDA review and labeling changes can take 6 to 18 months. The Sentinel system speeds this up by detecting patterns in real time, but validation still requires deep analysis to rule out other causes.
Why don’t doctors report side effects more often?
Time. Reporting a side effect to the FDA’s FAERS system takes about 22 minutes on average. Most doctors are overwhelmed with patient care and paperwork. Only 12% report consistently. Many don’t know how, or think their report won’t make a difference. But every report adds to the bigger picture.
Are newer drugs safer because of better data now?
Not necessarily. Newer drugs still start with limited trial data. But now, companies are required to plan for real-world monitoring from day one. So while initial safety profiles might still be incomplete, warnings come faster. Drugs like GLP-1 agonists had side effects flagged in real-world data within a year of launch-something that would have taken 5+ years a decade ago.
Should I stop taking my medication if I notice a side effect not on the label?
No. Don’t stop without talking to your doctor. But do track the symptom: when it happens, how bad it is, and what else you’re taking. Bring that info to your next appointment. Many side effects are manageable with dose changes or timing adjustments. Stopping suddenly can be dangerous. The goal is to find a balance-not to panic, but to act wisely.

June Richards on 1 February 2026, AT 14:54 PM
LMAO so now we're supposed to trust Reddit pharmacists over double-blind trials? 😂 Next thing you know, people will say vaccines cause autism because someone on TikTok felt tired after getting one.