When you're breastfeeding, every pill, injection, or patch you take doesn't just affect you. It can reach your baby through breast milk. That’s not something to panic about-but it is something to understand.
Most mothers assume that if a drug is safe for their baby to take directly, it’s safe through breast milk. That’s often true. But it’s not always that simple. Some medications cross into milk easily. Others barely make it through. And a few? They can build up over time and cause real problems.
The good news? Less than 2% of breastfed babies experience any serious side effects from medications in milk. The better news? You don’t have to stop breastfeeding just because you need medicine. In fact, fewer than 1% of all medications require you to stop nursing.
How Medications Get Into Breast Milk
It starts with your bloodstream. When you take a pill, the drug enters your blood. From there, it moves into the milk-producing cells in your breasts through a process called passive diffusion. Think of it like a sponge soaking up water-it follows the path of least resistance.
Not all drugs do this the same way. Four key things determine how much gets into your milk:
- Molecular weight: Drugs under 200 daltons slip through easily. Larger molecules, like heparin or insulin, mostly stay in your blood.
- Lipid solubility: Fatty drugs (like antidepressants or benzodiazepines) love to cross cell membranes. That means they show up more in milk.
- Protein binding: If a drug sticks tightly to proteins in your blood (over 90%), it can’t get into milk. Warfarin and most NSAIDs are like this-they barely make it through.
- Half-life: Drugs that stick around in your body longer (over 24 hours) have more time to build up in milk. Shorter half-life drugs like ibuprofen or amoxicillin clear out fast.
There’s also something called ion trapping. Breast milk is slightly more acidic than your blood. That traps weakly basic drugs-like lithium, certain antidepressants, or barbiturates-inside the milk. That’s why lithium levels in milk can be 2 to 10 times higher than in your blood. It doesn’t mean it’s unsafe, but it does mean you need to watch for signs of toxicity in your baby.
Right after birth, your milk is colostrum. It’s thick, sticky, and made in tiny amounts-only 30 to 60 milliliters a day. The gaps between your milk cells are wider then, so more drugs can slip through. But because your baby is drinking so little, the total dose they get is still very small. By day five, your milk volume increases, but the gaps close up. That’s when drug transfer becomes more predictable.
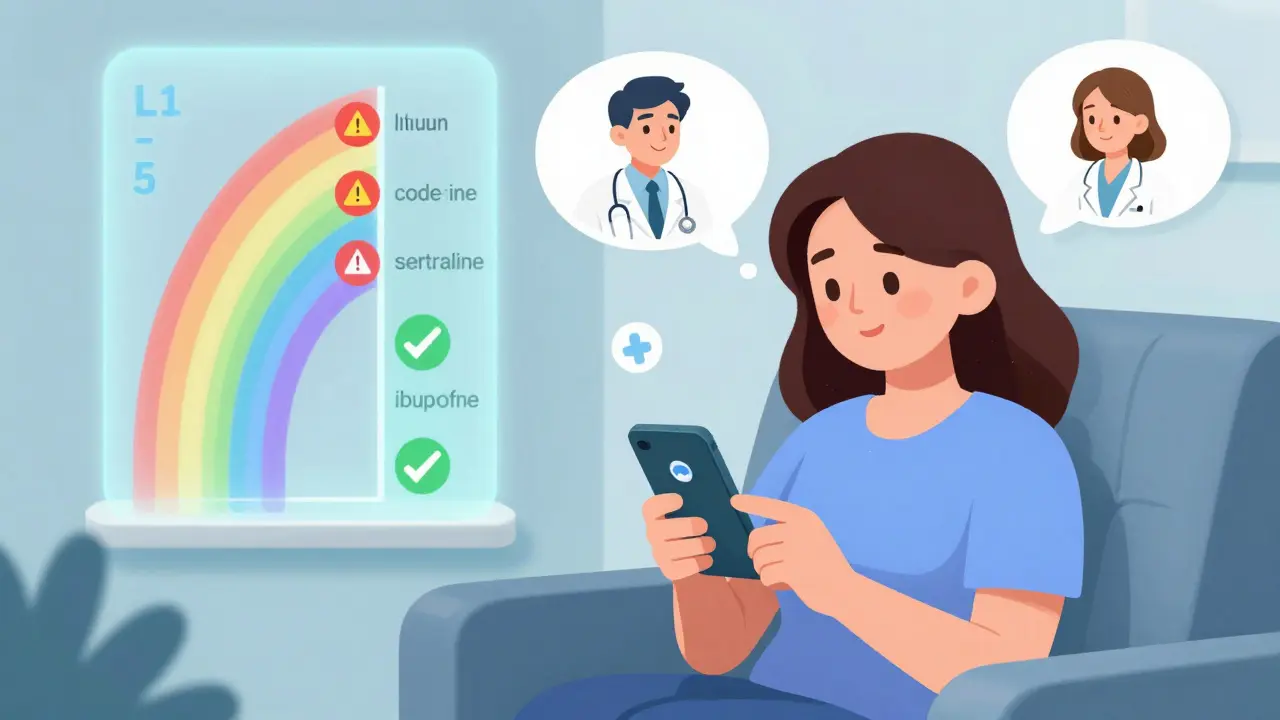
The L1 to L5 Risk System: What Your Doctor Should Be Using
Not all drugs are created equal when it comes to breastfeeding. Dr. Thomas Hale, a leading expert in this field, created a simple five-level system that’s used by doctors and lactation consultants worldwide.
Here’s what it means:
- L1: Safest - No documented risk. Examples: ibuprofen, amoxicillin, levothyroxine.
- L2: Probably Safe - Limited data, but no adverse effects reported. Examples: sertraline, ciprofloxacin, metformin.
- L3: Moderately Safe - Either limited human data or animal studies show risk, but benefits may outweigh risks. Examples: fluoxetine, gabapentin, cyclosporine.
- L4: Possibly Risky - Evidence of risk, but benefits may still justify use if no alternatives exist. Examples: lithium, methotrexate, some anticonvulsants.
- L5: Contraindicated - Proven risk. Don’t use. Examples: radioactive isotopes, chemotherapy drugs like doxorubicin, bromocriptine.
Most common medications-pain relievers, antibiotics, even many antidepressants-are L1 or L2. That means they’re safe to use while breastfeeding. You don’t need to pump and dump. You don’t need to switch to formula. You just need to know which ones are okay.
What Medications Are Most Commonly Used While Breastfeeding?
Studies show more than half of breastfeeding mothers take at least one medication. The top three categories?
- Analgesics (28.7%): Ibuprofen and acetaminophen are first-line. They’re safe, effective, and clear out quickly. Avoid aspirin and codeine-codeine can turn into morphine in your body and cause dangerous breathing issues in babies.
- Antibiotics (22.3%): Penicillins, cephalosporins, and macrolides like azithromycin are all L1 or L2. Even metronidazole is now considered safe in standard doses. Avoid tetracyclines for long-term use-they can stain baby’s teeth.
- Psychotropics (15.6%): Sertraline is the gold standard for depression and anxiety. It has the lowest transfer rate and the most safety data. Fluoxetine? Avoid if possible-it sticks around for weeks. Paroxetine is okay in low doses. For sleep, zolpidem is better than benzodiazepines.
Here’s a quick reference for common drugs:
| Medication | Use | Category (Hale) | Notes |
|---|---|---|---|
| Ibuprofen | Pain, fever | L1 | Low transfer, short half-life. Safe from day one. |
| Sertraline | Depression, anxiety | L2 | Best studied SSRI. Minimal infant exposure. |
| Amoxicillin | Antibiotic | L1 | Safe for newborns. May cause loose stools in baby. |
| Lithium | Bipolar disorder | L4 | Requires monitoring. Avoid in newborns. Use only if essential. |
| Codeine | Pain | L5 | Converts to morphine. Risk of fatal respiratory depression in infants. |
| Levothyroxine | Hypothyroidism | L1 | Essential for mom and baby. Safe at any dose. |

When and How to Take Medications to Protect Your Baby
Timing matters more than you think.
If you take a single daily dose, take it right after you breastfeed-especially before your baby’s longest sleep stretch. That gives your body time to clear the drug before the next feeding. For example, if your baby sleeps 6 hours at night, take your pill right after the 9 p.m. feeding. By 3 a.m., most of the drug is gone.
For multiple daily doses? Take them right before a feeding. That way, the drug level in your milk is lowest right before the next feed. This works especially well with short half-life drugs like ibuprofen or amoxicillin.
Topical creams? Generally safe-unless you’re putting them on your nipple. If you use a steroid cream on your breast, wash it off thoroughly before nursing. Same with nicotine patches-remove them during feedings if possible.
And here’s a tip most moms don’t know: if you’re on a medication that’s L3 or higher, ask your doctor about switching to one with lower lipid solubility, higher protein binding, or shorter half-life. Sometimes, there’s a safer alternative that works just as well.
What You Should Watch For in Your Baby
Most babies show no signs at all. But if your baby starts acting differently after you start a new medication, pay attention.
Watch for:
- Unusual sleepiness or fussiness
- Changes in feeding patterns (refusing feeds or feeding more often)
- Diarrhea or unusual stools
- Jaundice that doesn’t improve
- Slow weight gain
If you see any of these, don’t panic. But do call your pediatrician or lactation consultant. They can check if it’s the medication or something else.
And remember: just because a drug is in milk doesn’t mean it’s harmful. Babies are exposed to far more chemicals from the environment than from breast milk. The real danger comes from stopping breastfeeding because you’re scared.
Reliable Resources: What to Trust
Not every website is created equal. Google searches can give you scary, outdated, or wrong info.
Here are the only two resources you should use:
- LactMed (from the U.S. National Library of Medicine): Free, updated daily, covers over 4,000 drugs-including 350 herbs and supplements. It’s technical, but you can search by drug name and get detailed data on transfer rates, infant exposure, and alternatives. Over 1.2 million people use it every year.
- Medications and Mothers’ Milk by Dr. Thomas Hale: The go-to reference for clinicians. It uses the L1-L5 system and gives clear, practical advice. It’s not free, but many hospitals and clinics have copies.
Avoid websites that say “avoid all meds while breastfeeding” or “pump and dump for 24 hours.” That’s not evidence-based. It’s fear-based.
There’s also a new app called “LactMed On-the-Go,” which lets you search the database on your phone. It’s been downloaded over 45,000 times since 2023.
What’s Changing in 2025?
Science is catching up. In 2022, the FDA started pushing drug companies to include breastfeeding women in clinical trials. Before this, most new drugs had zero data on how they affect milk or babies.
Now, biologics-like Humira or Enbrel-are being studied. Only 12 out of 85 FDA-approved biologics had enough data in 2023. That’s changing fast.
And in the next five years, personalized medicine will start to enter this space. Researchers are already testing whether a mother’s genes can predict how fast she metabolizes a drug-and how much ends up in her milk. By 2030, we may be able to say: “Based on your genetics, sertraline is safe for you, but fluoxetine isn’t.”
The message? You’re not alone. You’re not doing something wrong. And you don’t have to choose between being a healthy mom and being a breastfeeding mom.
Medications and breastfeeding? They can work together. You just need the right information.
Is it safe to take ibuprofen while breastfeeding?
Yes. Ibuprofen is classified as L1-safest for breastfeeding. It has very low transfer into milk, a short half-life, and no reported side effects in breastfed infants. It’s the preferred pain reliever for nursing mothers.
Can antidepressants affect my baby’s development?
Sertraline, the most studied antidepressant for breastfeeding, shows minimal transfer and no negative impact on infant development, growth, or behavior in long-term studies. Other SSRIs like fluoxetine have higher transfer and longer half-lives, so they’re less ideal. Untreated depression, however, carries greater risks to both mother and child than medication exposure through milk.
Should I pump and dump after taking medication?
Almost never. Pumping and dumping doesn’t speed up drug clearance from your body-it just removes milk that already contains the drug. Unless you’re taking a truly dangerous medication (like chemotherapy), this practice is unnecessary and can hurt your milk supply. Timing your doses around feeds is far more effective.
Are herbal supplements safe while breastfeeding?
Not necessarily. Many herbs haven’t been studied for safety in breastfeeding. LactMed now includes data on 350 herbal products, but most have little to no safety data. Avoid high-dose supplements like sage (can reduce milk supply) or kava (linked to liver toxicity). Always check LactMed before using any herb or supplement.
What if my doctor says I have to stop breastfeeding?
Ask for a second opinion. A 2021 survey found that 78% of lactation consultants see at least one case per month where a mother was wrongly told to stop breastfeeding. Most medications are safe. If your doctor says to stop, ask them to consult LactMed or refer you to a lactation specialist. Your health and your baby’s health matter-both can be protected.
Next Steps: What to Do Today
If you’re on medication and breastfeeding:
- Check the drug’s category using LactMed or Hale’s guide. Don’t guess.
- Take your dose right after a feeding, especially before your baby’s longest sleep.
- Watch your baby for any unusual changes in behavior or feeding.
- If you’re unsure, talk to a lactation consultant-not just your doctor. They specialize in this.
- Remember: you’re not alone. Millions of mothers take meds and breastfeed safely every day.
There’s no reason to choose between your health and your baby’s. With the right knowledge, you can do both.


Meina Taiwo on 21 December 2025, AT 12:40 PM
Simple truth: if your med is on L1 or L2, keep nursing. No drama. LactMed is your friend. Done.