When someone is diagnosed with ALS, the focus quickly shifts from what’s coming next to what can be done now to hold onto quality of life. Two interventions stand out-not as cures, but as real, measurable ways to add months, sometimes years, to life while keeping people more alert, more comfortable, and more themselves. These are noninvasive ventilation (NIV) and proper nutrition management. They’re not optional extras. They’re core parts of care, backed by decades of research and real-world outcomes.
Why NIV Isn’t Just About Breathing
People often think of breathing problems in ALS as something that happens late, when the person is gasping for air. That’s not how it works. Respiratory decline starts quietly-morning headaches, trouble sleeping, feeling tired after a light meal, needing to prop yourself up with pillows to sleep. These aren’t normal aging signs. They’re signals that the diaphragm is weakening. Noninvasive ventilation doesn’t replace breathing. It supports it. A BiPAP machine delivers air pressure through a mask, helping the lungs inflate when the muscles can’t do it alone. Most people start with nighttime use, but as ALS progresses, many move to daytime use too. The goal isn’t just to survive-it’s to wake up feeling rested, think clearly, and stay out of the hospital. Studies show clear results. Without NIV, median survival after respiratory symptoms appear is about 215 days. With consistent use, that jumps to 453 days. That’s more than a year of extra life. And it’s not just about numbers. In ALS forums, 87% of users who stuck with NIV reported reduced morning headaches. Nearly 80% said their sleep improved. Over 70% felt more energy during the day.When to Start NIV-And Why Waiting Costs Time
There’s a dangerous gap between what guidelines say and what actually happens. The European and Canadian guidelines recommend starting NIV when forced vital capacity (FVC) drops below 80% or when symptoms like orthopnea or daytime sleepiness show up. That’s early. That’s smart. But in the U.S., many insurance companies won’t cover NIV unless FVC is below 50%, or sniff nasal inspiratory pressure (SNIP) is under 40 cm H₂O. That means people wait until they’re already struggling. By then, the muscles are too weak, the lungs too tired, and the body too compromised to adapt easily. The data doesn’t lie: starting NIV sooner leads to better outcomes. Patients who begin when FVC is still above 60% are more likely to tolerate the mask, adapt to the pressure, and use it for more than four hours a night-the threshold linked to survival benefit. Delaying NIV doesn’t delay the disease. It just delays the benefit.Choosing the Right Device
Not all ventilators are the same. Basic BiPAP machines cost $1,200-$2,500 and are great for nighttime use. But as ALS advances, many need more. That’s where devices like the Philips Respironics Trilogy 100 or 106 come in. These portable ventilators offer volume-assured pressure support (VAPS), dual backup rates, and built-in oxygen monitoring. They weigh less than 12 pounds. They have batteries that last 8-12 hours. That means you can use them while sitting in a chair, watching TV, or even taking a short walk outside. Users report higher satisfaction with these advanced devices. On ALS Toolkit reviews, the Trilogy scores 4.2 out of 5. Standard BiPAPs? 3.7. Why? Because comfort matters. If the machine feels like a burden, you won’t use it. And if you don’t use it, you lose the benefit.
Mask Fit and Adherence-The Real Battle
The biggest reason people quit NIV isn’t the machine. It’s the mask. Skin breakdown, air leaks, claustrophobia, difficulty exhaling against pressure-these are real problems. In one study, 63% of non-adherent patients cited mask discomfort. Over 40% had sores on their nose or face. But here’s the good news: these issues are fixable. A good respiratory therapist doesn’t just hand you a mask and say, “Try this.” They spend time-often 1.5 hours per session-adjusting straps, trying different cushion types (silicone, gel, nasal pillows), and teaching breathing techniques. They check for pressure points. They adjust IPAP and EPAP settings. Initial settings? Usually IPAP 12-14 cm H₂O, EPAP 4-6 cm H₂O, with a backup rate of 12 breaths per minute. Then they tweak based on blood gases and how the person feels. Adherence improves over time. In the first 30 days, people use NIV an average of 20 days. By one year? That jumps to 27.5 days per month. Support makes the difference.Nutrition: It’s Not About Eating More-It’s About Eating Sustainably
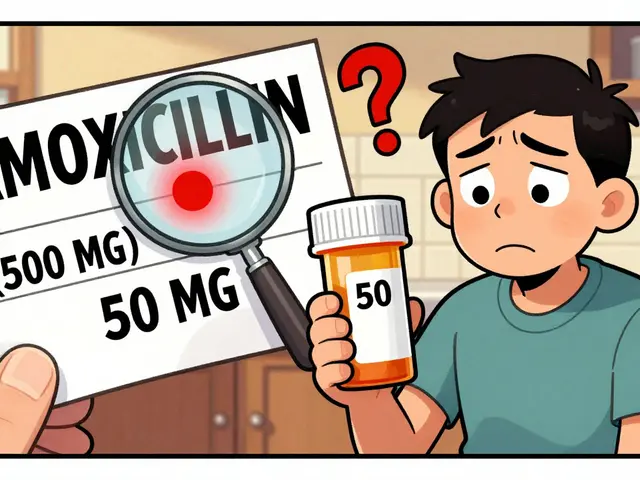
Swallowing problems in ALS don’t come out of nowhere. They creep in. You start avoiding crunchy foods. You take longer to finish meals. You cough after drinking water. These aren’t just inconveniences. They’re red flags. Weight loss in ALS isn’t normal. It’s dangerous. Losing more than 5% of your body weight in six months is linked to faster decline and shorter survival. The goal isn’t to gain weight. It’s to stop losing it. That’s where percutaneous endoscopic gastrostomy (PEG) tubes come in. A PEG tube is a small tube placed directly into the stomach through the abdomen. It’s not a last resort. It’s a tool to keep nutrition stable. The AAN recommends placing it before FVC drops below 50% or BMI falls under 18.5 kg/m². Why? Because once the lungs are too weak, surgery becomes riskier. One study showed that without a PEG, ALS patients lost an average of 12.6% of their body weight in six months. With a PEG? Just 0.5%. That’s not a small difference. That’s life versus decline. PEG doesn’t mean you stop eating by mouth. Most people still enjoy small meals for taste and social reasons. The tube just ensures they get enough calories and protein-even on days when swallowing is hard.Putting It All Together
ALS care isn’t about one treatment. It’s about timing, coordination, and consistency. When NIV and PEG are both introduced early and supported properly, the survival advantage isn’t 7 months or 120 days. It’s over 12 months. A 2021 multinational registry analysis found that people who received both interventions had a median survival advantage of 12.3 months compared to those who got neither. That’s not a guess. That’s data from thousands of patients across multiple countries. The key isn’t waiting for crisis. It’s acting before the crisis hits. Counseling on NIV should happen within 30 days of FVC dropping below 80% or the first symptom of respiratory trouble. PEG should be discussed as soon as swallowing changes appear-not when choking becomes frequent.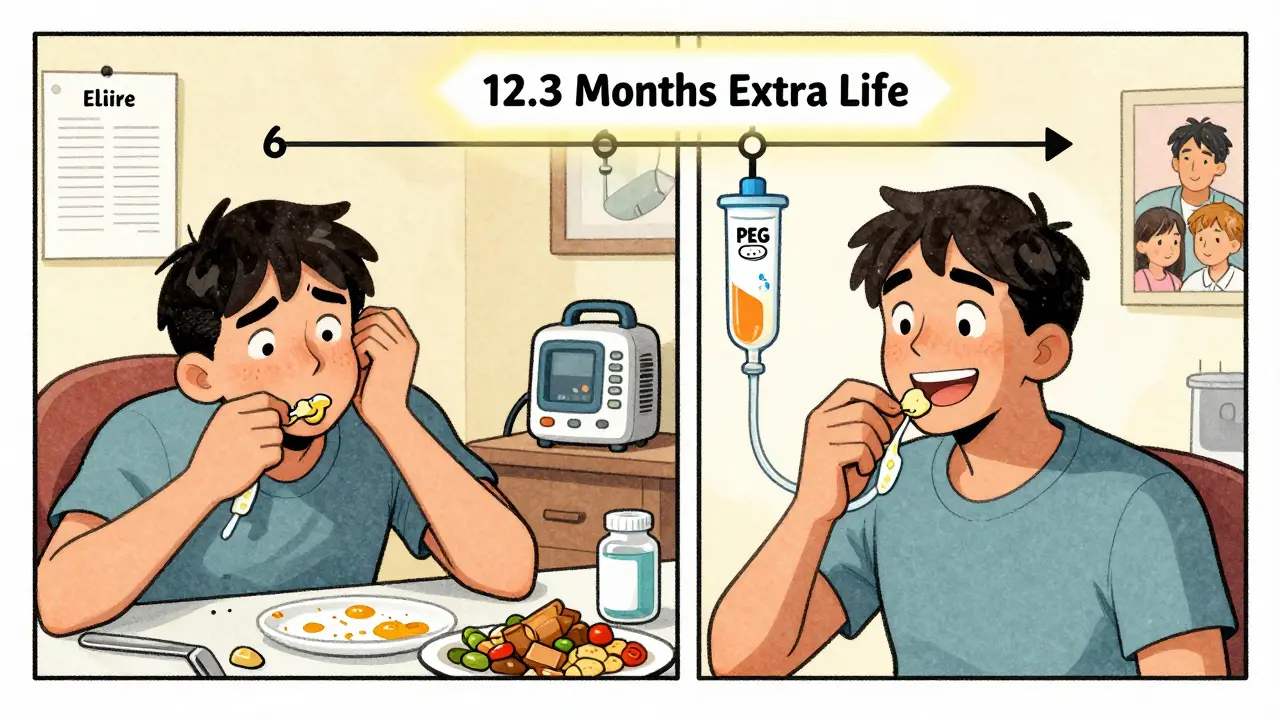
What Doesn’t Work
Some still believe NIV is only for people without bulbar symptoms. That’s outdated. A 2013 study showed patients with bulbar involvement (difficulty speaking or swallowing) benefit just as much as those without. NIV doesn’t worsen aspiration risk. In fact, better breathing can improve cough strength and reduce secretions. Others think nutrition means high-calorie shakes or supplements. But it’s not about quantity-it’s about consistency. A person on a PEG tube needs balanced nutrition: protein to maintain muscle, fiber to prevent constipation, fluids to avoid dehydration. A dietitian specializing in ALS makes all the difference.What Comes Next
Research is moving faster. Trials like NCT07071935 are testing predictive algorithms to guess who’ll need NIV before symptoms appear. Others are looking at real-time CO₂ monitoring to adjust ventilation automatically. Wearable sensors might soon alert care teams when a patient’s nighttime breathing drops below safe levels. But for now, the tools we have work. And they work best when used early, with support, and without delay.Can you use NIV during the day, or just at night?
Yes, many people use NIV during the day as ALS progresses. While most start with nighttime use, devices like the Philips Trilogy 100/106 are portable, battery-powered, and designed for daytime use. Daytime NIV helps reduce fatigue, improve concentration, and prevent worsening hypercapnia. It’s not a sign of decline-it’s a tool to maintain function.
Does a PEG tube mean you can’t eat by mouth anymore?
No. A PEG tube supplements nutrition, not replaces it. Most people continue eating small amounts of food they can swallow safely. Eating by mouth helps maintain taste, social connection, and oral motor function. The tube ensures they get enough calories and protein when swallowing becomes too tiring or risky.
How do you know if NIV is working?
There are clear signs: fewer morning headaches, better sleep, more energy during the day, and less shortness of breath. Clinically, doctors check blood gases-targeting PaCO₂ below 45 mmHg and SpO₂ above 92% during sleep. Device download data showing usage over 4 hours per night is the strongest predictor of survival benefit.
Is NIV covered by insurance?
Coverage varies. Medicare and many private insurers cover NIV if criteria like FVC <50%, SNIP <40 cm H₂O, or MIP <-60 cm H₂O are met. But guidelines recommend starting earlier-when symptoms appear or FVC drops below 80%. Some families work with ALS care centers to appeal denials using clinical evidence and specialist letters.
What if someone can’t tolerate a mask?
There are options. Different mask types-nasal pillows, full face, hybrid-can make a big difference. Adjusting pressure settings, using a humidifier, or trying a ramp feature that slowly increases pressure can help. Many patients need multiple visits with a respiratory therapist to find the right fit. Persistence pays off: adherence improves significantly after the first month with proper support.
Can you still travel with NIV or a PEG tube?
Yes. Portable ventilators like the Trilogy have built-in batteries and work on airplane power. PEG tubes don’t restrict travel-many people travel with feeding supplies in coolers or use ready-to-hang formulas. It’s important to plan ahead with medical providers, carry documentation, and know where to get supplies at your destination. Most airlines and travel insurers are familiar with these devices.


Janette Martens on 30 December 2025, AT 06:29 AM
why the hell are we even talking about this like it's a miracle? NIV and PEG are just band-aids on a bullet wound. ALS kills you slow and the system knows it. They push these tools because it's cheaper than real research. I'm from Canada and we're sold this crap as 'compassionate care' but really it's just prolonging suffering so hospitals don't lose bed space.