Drug shortages aren’t just inconvenient-they’re life-threatening. When a critical antibiotic or heart medication runs out, hospitals scramble. Patients delay treatment. Some die. The problem isn’t random. It’s systemic. And it’s getting worse. In 2025, the U.S. still produces only 28% of its essential medicine active pharmaceutical ingredients (APIs) domestically. For sterile injectables, that number drops to 12%. Antibiotics? Just 17%. The rest comes from overseas-mostly China and India, which together make up 68% of global API production.
Why Resilience Isn’t Optional Anymore
The old model-lean, global, cost-optimized-collapsed during COVID-19. Suddenly, the world realized that relying on a single factory in a distant country for a life-saving drug was a gamble no one should take. The U.S. Department of Defense called pharmaceutical supply chain gaps a critical national security risk. The FDA confirmed that 80% of APIs and 40% of finished drugs in America are made abroad. When geopolitical tensions rise, shipping delays hit, or a factory shuts down, the ripple effect reaches every pharmacy shelf. Resilience isn’t about being immune to disruption. It’s about surviving it. The Mathematica Inc. report from 2023 defined it clearly: the ability to anticipate, prepare for, respond to, and recover from disruptions while keeping critical drugs flowing. That’s not a luxury. It’s a public health necessity.Three Pillars of a Resilient Supply Chain
Building resilience isn’t one fix. It’s three interconnected systems working together: preparedness, response, and recovery. Preparedness means knowing where your vulnerabilities are. Leading companies now map out 12 to 15 tiers of suppliers-not just their direct vendors, but their vendors’ vendors. They track where APIs come from, what raw materials are used, and which logistics routes are most fragile. One major pharma firm found that a single dye supplier in Turkey was blocking production of a cancer drug because the dye was critical for labeling. No one had checked that far down the chain. Response is about having options ready. Companies that dual-source 70-80% of their critical components cut disruption time in half. If one API plant in India goes offline, they switch to another in Germany or Mexico. Buffer stocks help too. Keeping 60 to 90 days of inventory for essential medicines isn’t wasteful-it’s insurance. The FDA’s new Strategic Active Pharmaceutical Ingredients Reserve aims to stockpile 90-day supplies of 150 critical drugs by 2027. That’s a start. Recovery means bouncing back fast. That’s where new manufacturing tech comes in. Traditional batch production takes years to set up and is rigid. Continuous manufacturing, on the other hand, can be scaled up in months. These modular, container-based systems can go from zero to 50kg of API production in under a year. They use 30-40% less space, 20-25% less energy, and waste 15-20% less material. The catch? They cost $50-150 million to build-three to five times more than a batch facility. Only 12 such systems have been approved by the FDA as of mid-2025, out of over 10,000 batch approvals. The regulatory system is lagging behind the tech.Technology Is Changing the Game
AI isn’t just hype in pharma supply chains-it’s saving lives. Companies using AI for demand forecasting and disruption prediction now see 85-90% accuracy in spotting risks 60 to 90 days ahead. One firm caught a potential shortage of a diabetes drug because AI flagged rising freight costs from a port in Shanghai three months before shipments slowed. They reordered early, avoided the shortage, and kept patients covered. Blockchain is another quiet hero. Pilots in Europe and the U.S. show it can reduce counterfeit drugs by 70-75%. When every pill’s journey-from raw chemical to patient’s hand-is tracked on an immutable ledger, fake meds can’t slip through. That’s huge. Counterfeit drugs kill an estimated 1 million people globally each year. But tech alone won’t fix this. Data silos still plague the industry. A 2024 PwC survey found that 65% of pharma companies can’t connect their inventory data with supplier data or logistics info. Without integrated systems, even the best AI can’t see the full picture.Where the U.S. Stands-and What’s Being Done
The U.S. government is finally stepping in. In August 2025, an executive order created the Strategic Active Pharmaceutical Ingredients Reserve. It’s not just symbolic-it’s funded. $1.2 billion from the CHIPS and Science Act, plus $800 million more proposed in the 2025 budget, is going toward building domestic API capacity. The goal? Raise domestic production from 28% to 35-40% by 2030. But here’s the problem: you can’t just “onshore everything.” The CSIS report in 2025 made it clear: trying to bring every single API back to the U.S. is impossible. The cost would spike by 20-30%, and you’d just replace one vulnerability with another-like depending on one U.S. factory instead of two in India and one in Germany. The smarter path? Regionalization. Build manufacturing networks across North America, Europe, and Asia-Pacific. Diversify. Don’t isolate. North American companies have already cut China-sourced APIs from 38% in 2022 to 29% in 2025. They’re shifting to Mexico, Canada, and Eastern Europe. That’s the model: not isolation, but balance.The Real Cost of Doing Nothing
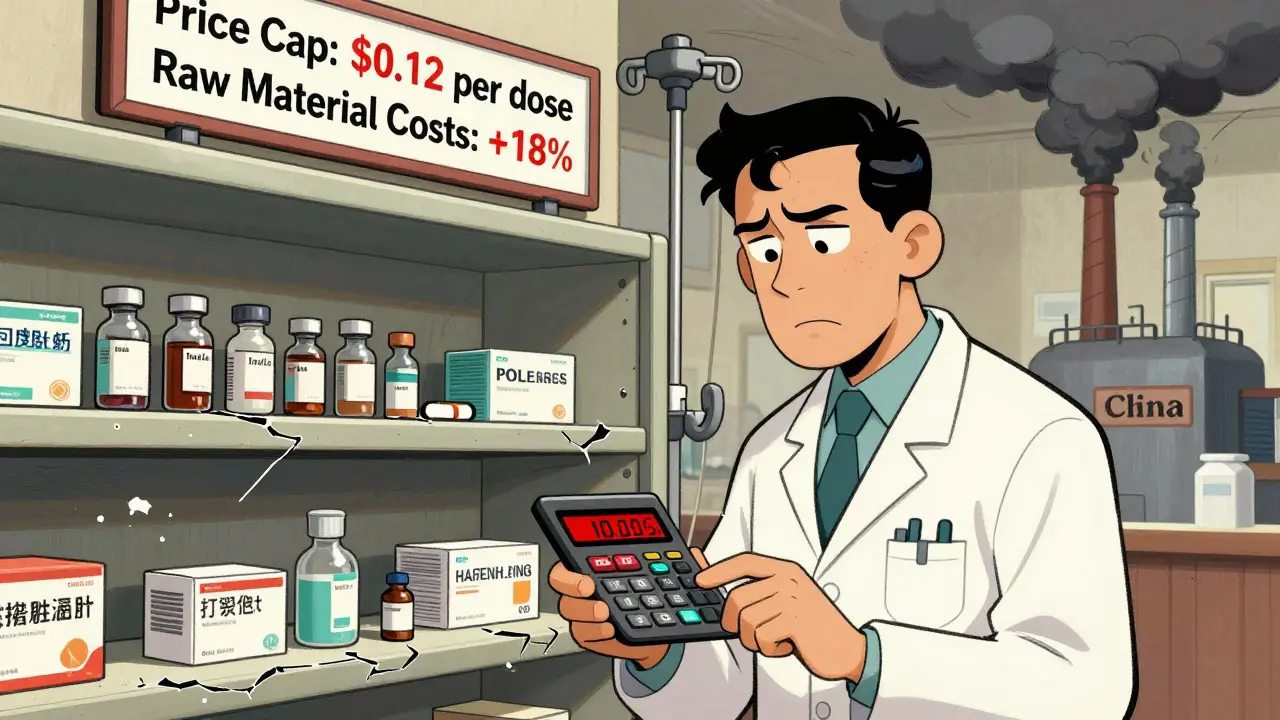
Some executives say, “Why spend more when we’ve gotten by?” But the math doesn’t lie. ZS Associates found that companies with full resilience strategies had 23% higher operational continuity during disruptions. That translates to $14.7 million saved per major event in avoided lost sales, emergency imports, and legal liabilities. Smaller companies are falling behind. Only 18% of small pharma firms (<$1 billion revenue) have any formal resilience plan. Mid-sized firms? 42%. Big players? 85%. That gap isn’t just unfair-it’s dangerous. When a small manufacturer can’t secure APIs, the entire supply chain feels it. Investing in resilience adds 8-12% to the cost of goods sold. But the return? PwC says 1.8x ROI within three years. That’s not a cost center. It’s a profit protector.
What Works in Practice
The best strategies follow a clear path:- Assess every supplier tier-go beyond your direct vendors.
- Map your critical products: which ones cause the most harm if they disappear?
- Diversify sourcing for at least 70% of those critical items.
- Stock 60-90 days of inventory for top-priority drugs.
- Invest in tech: AI for forecasting, blockchain for traceability.
- Train teams with real-world disruption scenarios-once a year isn’t enough.
- Align legal, procurement, manufacturing, and logistics under one resilience leader.
The Road Ahead
By 2027, 45-50% of new manufacturing capacity will use continuous production. By 2030, regional networks will supply 65-70% of U.S. needs. But we’re not there yet. Workforce shortages loom. The U.S. will need 250,000 more skilled manufacturing workers by 2027. Regulatory standards still don’t match across countries-only 35% of manufacturing rules are aligned globally. And the global investment needed to fix this? $120-150 billion. The solution isn’t a single policy, a new factory, or a tariff. It’s a mix: smart tech, diversified sourcing, strategic stockpiles, and leadership that treats supply chains like infrastructure-not an expense line. The next drug shortage won’t be an accident. It’ll be a failure of preparation. And we’ve had enough of those.What are the biggest causes of drug shortages today?
The top causes are foreign manufacturing disruptions (especially in China and India), raw material shortages, regulatory delays, and single-source dependencies. A single factory shutdown for quality issues can halt production of a drug used by millions. Geopolitical tensions and shipping bottlenecks also play a major role.
How much inventory should a hospital keep for critical drugs?
For essential medicines like antibiotics, insulin, or heart drugs, experts recommend 60 to 90 days of inventory. That’s not excessive-it’s a buffer against delays. Many hospitals keep only 30 days or less, which leaves them vulnerable during supply chain shocks.
Is onshoring all drug manufacturing the answer?
No. Trying to bring every API back to the U.S. would raise costs by 20-30% and create new risks, like over-reliance on one domestic plant. The smarter approach is regional diversification: building capacity in North America, Europe, and other stable regions to balance cost, speed, and risk.
Can AI really predict drug shortages before they happen?
Yes. Leading companies using AI-powered forecasting tools can predict disruptions with 85-90% accuracy up to 90 days in advance. These systems analyze shipping data, weather patterns, political events, supplier financial health, and even social media chatter about raw material shortages.
Why aren’t more companies investing in resilience?
Three main reasons: short-term cost pressure, lack of executive buy-in, and fragmented data systems. Many CFOs see resilience as an expense, not an investment. Without leadership pushing it, departments don’t coordinate. And if inventory, procurement, and logistics systems don’t talk to each other, no plan works.
What’s the role of the FDA in improving supply chain resilience?
The FDA is speeding up approvals for continuous manufacturing and launching the Strategic Active Pharmaceutical Ingredients Reserve. They’re also working to harmonize global standards and increasing inspections of foreign facilities. But they can’t fix the supply chain alone-they need industry cooperation and government funding to scale solutions.

Andrew Forthmuller on 11 November 2025, AT 21:21 PM
this is wild. we’re literally gambling with people’s lives over cheaper pills. how did we let this happen?