Getting prescribed a medication you can’t afford is a common problem - and it’s not your fault. In 2024, nearly 3 in 10 Americans skipped doses or didn’t fill prescriptions because of cost. But there’s a proven way to cut your bill without sacrificing effectiveness: asking for a therapeutic alternative. This isn’t about generics or coupons. It’s about swapping one medication for another that works just as well - but costs a fraction of the price.
What Is a Therapeutic Alternative?
A therapeutic alternative isn’t the same as a generic. Generics are chemically identical to brand-name drugs. A therapeutic alternative is a different drug - often from the same class - that treats the same condition with similar results. For example:- Instead of esomeprazole (Nexium), you might take omeprazole - same effect, 96% cheaper.
- Instead of Lyrica (pregabalin), your doctor might suggest gabapentin - both treat nerve pain, but gabapentin costs $15/month vs. $450.
- Instead of Eliquis, you could switch to warfarin - saving up to $450 a month.
These swaps aren’t guesses. They’re backed by clinical studies showing comparable safety and effectiveness. A 2017 study from Vanderbilt University found that switching to therapeutic alternatives saved patients an average of $17.77 per person per month - with no drop in health outcomes.
Why Don’t Doctors Always Suggest This?
Many doctors know about therapeutic alternatives. But they don’t always bring them up. Why? Here’s the reality:- They’re busy. A 10-minute appointment leaves little room for cost discussions.
- They’re used to prescribing what’s on the formulary. Insurance lists often push brand-name drugs, even when cheaper options exist.
- They worry about effectiveness. Some doctors fear that even small differences in drugs could hurt patients - and they’re right to be cautious in some cases.
But here’s the key: you don’t need to wait for your doctor to bring it up. You can start the conversation.
How to Ask for a Lower-Cost Alternative
This isn’t about arguing. It’s about asking the right way. Follow these steps:- Start with cost. Say: "I’m having trouble affording this medication. Are there other options that work just as well but cost less?" This opens the door without sounding confrontational.
- Do your homework. Use GoodRx or NeedyMeds to check prices. If you find a cheaper drug that treats the same condition, bring it up. Example: "I saw that gabapentin costs $15 a month for nerve pain. Is that something we could try?"
- Know the difference between generics and therapeutic alternatives. If your drug has no generic, ask: "Is there another drug in the same class that’s cheaper?" For example, if you’re on Crestor (rosuvastatin), ask about atorvastatin - same cholesterol-lowering effect, often 80% cheaper.
- Ask about extended prescriptions. A 90-day supply often cuts your copay by 25%. Ask: "Can I get a 90-day supply to lower my monthly cost?"
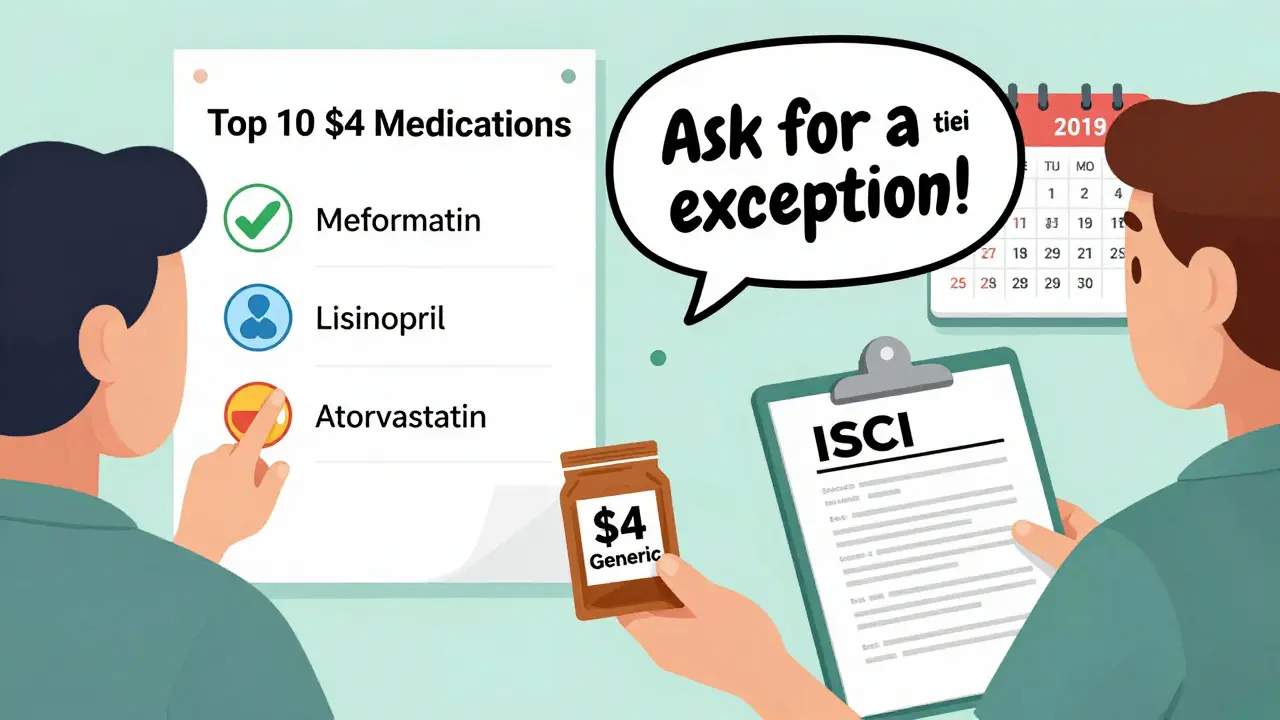
- Request a tiering exception. If your insurance denies coverage for a cheaper drug, ask your doctor to file a "tiering exception." This is a formal request to cover a non-preferred drug at a lower cost. Medicare Part D must respond within 72 hours for urgent cases.

When Therapeutic Alternatives Don’t Work
Not every drug has a good alternative. About 15% of specialty medications - especially for cancer, autoimmune diseases, or rare conditions - have no comparable substitutes. In those cases, you’ll need other strategies:- Manufacturer copay cards. Companies like Pfizer, AbbVie, and Janssen offer cards that can cut your bill to $0 for brand-name drugs. Visit their websites or ask your pharmacist.
- Patient assistance programs. Programs like NeedyMeds, RxAssist, and the HealthWell Foundation help low-income patients. Eligibility is usually based on income under $60,000/year for individuals.
- State pharmacy discount programs. Walmart, CVS, and Walgreens offer $4 lists for common generics: lisinopril, metformin, atorvastatin, levothyroxine. These are often cheaper than insurance copays.
One patient switched from Jardiance to metformin and found their blood sugar worsened. That’s why therapeutic alternatives aren’t one-size-fits-all. But for most chronic conditions - high blood pressure, diabetes, cholesterol, acid reflux, depression - there’s a cheaper option that works.
Real Savings, Real Stories
People are saving hundreds a month with these swaps:- One person saved $380/month switching from Crestor to atorvastatin.
- A patient with atrial fibrillation cut their bill from $450 to $15/month by switching from Eliquis to warfarin.
- A woman with GERD went from $365/month for esomeprazole to $15 for omeprazole.
These aren’t outliers. A 2024 GoodRx survey of 12,500 patients found that 68% successfully switched to a cheaper therapeutic alternative. The average monthly savings? $47.25. Multiply that by 12 months - that’s over $500 saved per year, just from one conversation.
What to Do If Your Doctor Says No
Sometimes, doctors hesitate. They might say: "This drug is better for you," or "The other one doesn’t work as well." Here’s how to respond:- Ask for evidence. "Can you show me the data showing this drug is significantly better than the alternative?" Most of the time, they can’t.
- Request a trial. "Could we try the cheaper option for 30 days? If it doesn’t work, we can switch back."
- Get a second opinion. Talk to your pharmacist. They know drug equivalencies better than most doctors. Many pharmacies have clinical pharmacists on staff who can help you make the case.
- Use official guidelines. Print out the Institute for Clinical Systems Improvement guidelines for your condition. They list approved therapeutic alternatives for over 125 conditions.
One patient brought a printed guideline showing that gabapentin was clinically equivalent to pregabalin for neuropathic pain. Her neurologist agreed to the switch - and saved her $435 a month.
What’s Changing in 2026
The system is slowly improving:- Electronic health records like Epic and Cerner now flag therapeutic alternatives at the point of prescribing. Doctors get a one-click suggestion: "Consider atorvastatin instead of rosuvastatin - saves $320/month."
- Medicare Part D now requires all plans to use standardized criteria for therapeutic interchange. If your doctor says a cheaper drug is appropriate, your insurer must approve it quickly.
- AI tools are being tested to predict which patients would benefit from a switch. One 2024 study found AI identified 89% of good therapeutic alternatives - better than human doctors.
But the biggest change? More patients are speaking up. In 2019, only 22% of patients asked about cost. By 2025, that number jumped to 58%. You’re not alone. And you’re not being difficult. You’re being smart.
Final Checklist: Your Action Plan
Here’s what to do next:- Write down every medication you take - including dose and frequency.
- Check prices on GoodRx or NeedyMeds for each one.
- Find cheaper alternatives in the same drug class.
- Call your pharmacy - ask if they offer a $4 generic list.
- Book an appointment with your doctor and say: "I want to talk about lowering my medication costs. Can we review my prescriptions?"
- Bring printed info - a GoodRx screenshot or a page from NeedyMeds.
- Ask for a 90-day supply - it’s often cheaper per pill.
- Ask about copay cards or patient assistance programs.
You don’t need to be an expert. You just need to ask. And if your doctor resists? Keep asking. Your health - and your wallet - depend on it.
What’s the difference between a generic and a therapeutic alternative?
A generic is the exact same chemical as the brand-name drug, just cheaper. A therapeutic alternative is a different drug - often from the same class - that treats the same condition with similar results. For example, omeprazole and esomeprazole are both proton pump inhibitors, but they’re chemically different. One can be 96% cheaper than the other.
Can I switch to a cheaper drug on my own?
No. Never stop or switch medications without talking to your doctor. Even if a drug seems similar, stopping abruptly or switching without guidance can be dangerous. Always get approval first.
What if my insurance won’t cover the cheaper drug?
Ask your doctor to file a "tiering exception." This is a formal request to cover a non-preferred drug at a lower cost. For Medicare Part D, insurers must respond within 72 hours for urgent cases. If they deny it, you can appeal.
Are therapeutic alternatives safe?
Yes - when chosen properly. Studies show that for conditions like high blood pressure, diabetes, and acid reflux, therapeutic alternatives have the same effectiveness and safety as brand-name drugs. But they’re not right for everyone. Your doctor should consider your age, other medications, and medical history before switching.
How do I find out if a cheaper alternative exists?
Use GoodRx or NeedyMeds. Enter your medication name, and it will show you cheaper options in the same drug class. You can also ask your pharmacist - they know which drugs are clinically interchangeable.
Can I use GoodRx even if I have insurance?
Yes. Sometimes GoodRx prices are lower than your insurance copay. Always compare. You can use GoodRx instead of insurance - or sometimes combine them. Ask your pharmacist to run both options.
What if my doctor says there’s no cheaper option?
Ask them to check the Institute for Clinical Systems Improvement guidelines. Many drugs have approved alternatives that even doctors overlook. Also, ask if you can try a 30-day trial of a cheaper option - if it doesn’t work, you can switch back.
Do therapeutic alternatives work for mental health medications?
Yes. For depression, switching from brand-name Lexapro to generic escitalopram saves money. For anxiety, switching from Xanax to generic alprazolam works the same. But mood stabilizers and antipsychotics are trickier - always consult your psychiatrist before switching.


evelyn wellding on 16 January 2026, AT 14:57 PM
OMG THIS IS LIFE-CHANGING 😭 I was paying $400/month for Eliquis and just switched to warfarin with a co-pay card-now it’s $12! My bank account is crying happy tears. 🙌