SSRI Sexual Side Effect Management Tool
Your Situation
Recommended Approach
Answer your situation questions above to see personalized recommendations.
Key Considerations
Efficacy
Onset
*Based on current evidence for bupropion adjunct therapy
When you’ve finally found an SSRI that eases your depressive symptoms, only to discover that your sex life has taken a hit, the frustration can feel overwhelming. SSRI sexual dysfunction isn’t a rare quirk - studies show 35‑70 % of patients on these drugs notice reduced libido, delayed orgasm, erectile problems, or trouble with arousal within the first month of treatment. The good news? You don’t have to choose between mood stability and satisfying intimacy. Below is a step‑by‑step playbook that walks you through assessment, dosage tweaks, medication switches, and proven adjuncts so you can reclaim both mental health and sexual wellbeing.
What Exactly Is SSRI‑Induced Sexual Dysfunction?
SSRI‑induced sexual dysfunction is a side‑effect profile that includes reduced libido (≈40‑50 % of cases), delayed or absent orgasm (≈60‑70 %), erectile dysfunction (≈20‑30 %), and impaired arousal or lubrication (≈40‑50 %). It typically emerges within 2‑4 weeks of starting an SSRI, as documented by Montejo et al. (2019). The condition can be hard to spot because 35‑50 % of people with major depression already experience some degree of sexual difficulty before any medication is prescribed (Harvard Health, 2023).
Why does it happen? Serotonin excess dampens dopamine pathways that drive sexual desire and response. In practical terms, the medication that lifts your mood can simultaneously press the brake on the pleasure circuit.
Step 1: Early Assessment & Ongoing Monitoring
The first 2‑4 weeks are critical. Schedule a brief check‑in at week 2 and again at week 4 using a standardized tool such as the Arizona Sexual Experience Scale (ASEX) or the Antidepressant Sexual Dysfunction Inventory. Ask direct, non‑judgmental questions: "How's your desire? Any trouble reaching climax?" Research shows that patients who are proactively screened are far more likely to stay adherent to treatment (Montejo et al., 2019).
Document the baseline at initiation - note the specific SSRI, dose, and any pre‑existing sexual concerns. Repeat the same scale each visit; a 10‑point change on ASEX usually reflects a clinically meaningful shift.
Step 2: Dose Modification Strategies
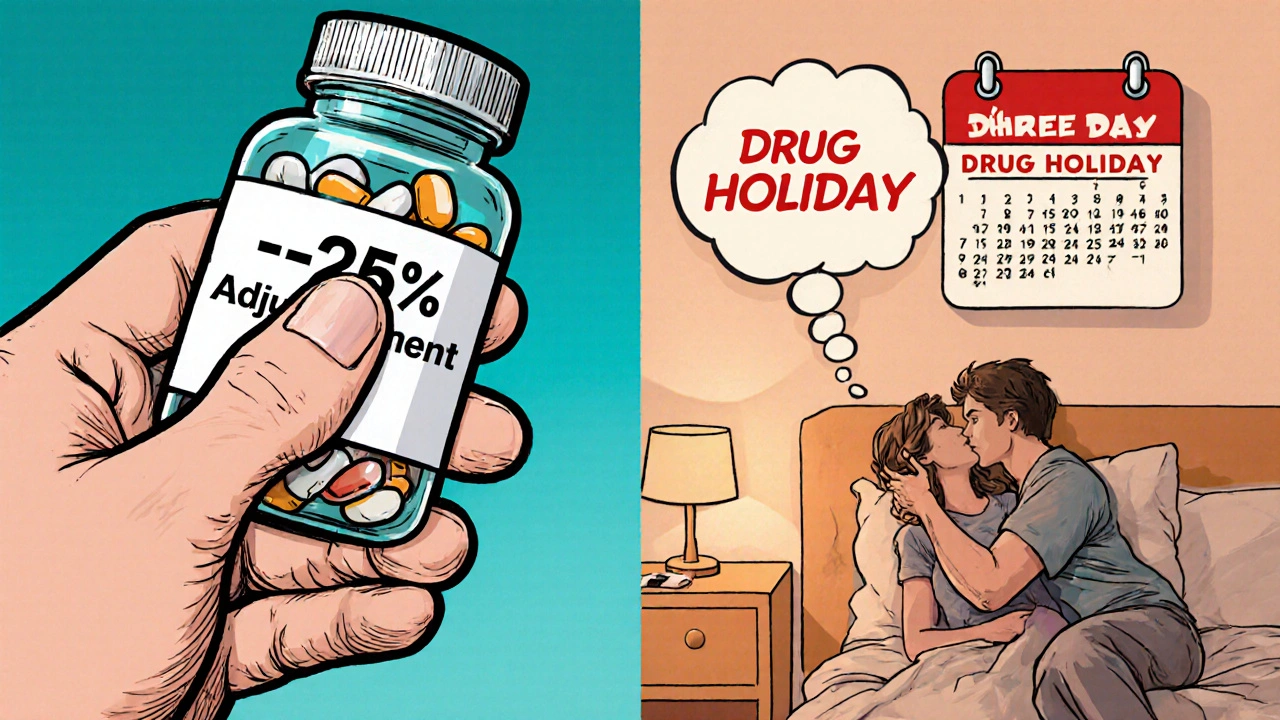
If the side effect is mild‑to‑moderate, the simplest move is to adjust the dose. Chapleau et al. (2023) found that a 25‑50 % dose reduction improves sexual function in 40‑60 % of patients while preserving antidepressant efficacy for mild‑to‑moderate depression.
- Dose reduction: Lower the daily dose by a quarter to a half. Re‑evaluate after 2 weeks.
- Drug holiday: Skip the SSRI for 48‑72 hours before planned sexual activity - works only for short‑half‑life agents like sertraline or citalopram. Fluoxetine’s half‑life exceeds 14 days, making holidays ineffective.
Evidence from Montejo’s non‑controlled study (30 participants) showed 60‑70 % improvement in anorgasmia with short‑half‑life agents when a drug holiday was used. Beware of discontinuation syndrome - 15‑20 % of patients report dizziness, nausea, or anxiety during the off‑days.
Step 3: Switching to a Different Antidepressant
When dose tweaks don’t help, consider a switch. Not all SSRIs are equal:
- Sertraline and Fluoxetine have relatively lower sexual side‑effect rates than paroxetine (Jing et al., 2016).
- Switching to bupropion, a norepinephrine‑dopamine reuptake inhibitor, resolves sexual dysfunction in 60‑70 % of cases. Titration takes 2‑4 weeks to avoid mood destabilisation.
- Mirtazapine or nefazodone (5‑HT2A antagonists) improve dysfunction in 50‑60 % but cause sedation in 30‑40 % of patients.
Switching to bupropion carries a relapse risk of 25‑30 % in severe depression, versus 10‑15 % when staying on the original SSRI (Montejo, 2019). Weigh that against the impact of persistent sexual problems on quality of life.
Step 4: Adjunct Pharmacotherapies - Adding a Helper
Adjuncts have the strongest evidence base. The most studied is bupropion, either as a daily augmentation or taken an‑as‑needed dose before intimacy.
- Daily SR‑bupropion 150 mg twice a day yielded a 66 % improvement in desire and frequency (Jing et al., 2016, p=.024).
- Immediate‑release 75 mg taken 1‑2 hours before sex improved symptoms in 38 % of patients.
Other options include:
- Ropinirole (dopamine agonist, 0.25‑1 mg daily) - 40‑50 % efficacy but may cause anxiety and tremor.
- Amantadine (100 mg daily) - similar efficacy, same side‑effect caveats.
- Buspirone (5‑15 mg daily) - 45‑55 % response, low discontinuation (5‑10 %).
- Cyproheptadine (2‑4 mg as needed) - 50 % success, but sedation in 35‑40 %.
All adjuncts carry a theoretical 5‑8 % chance of reducing the primary antidepressant’s efficacy when not carefully managed.
Comparing Management Options
| Strategy | Typical Efficacy (% improvement) |
Onset | Key Risks |
|---|---|---|---|
| Dose reduction | 40‑60 | 2‑4 weeks | Potential mood relapse if dose too low |
| Drug holiday (short‑half‑life) | 60‑70 (anorgasmia) | 48‑72 hours | Discontinuation syndrome (15‑20 %) |
| Switch to bupropion | 60‑70 | 2‑4 weeks titration | Relapse risk 25‑30 % in severe cases |
| Daily bupropion adjunct | 66 | 3‑4 weeks | Increased anxiety 20‑25 % |
| As‑needed bupropion | 38 | 1‑2 hours pre‑sex | Less consistent benefit |
| Dopaminergic agents (ropinirole, amantadine) | 40‑50 | 48‑72 hours | Anxiety, tremor (≈30 %) |
| Serotonergic modulators (buspirone, cyproheptadine) | 45‑55 | 2‑3 weeks | Sedation (35‑40 % for cyproheptadine) |

Choosing the Right Approach for You
Think of decision‑making as a flow chart:
- Is the sexual issue mild and not distressing? Try dose reduction first.
- Do you use a short‑half‑life SSRI and have predictable sexual timing? A drug holiday may be the quickest fix.
- Is the dysfunction severe or persistent after 4 weeks? Consider switching to bupropion or another low‑impact antidepressant.
- Prefer to stay on your current SSRI? Add an adjunct - daily bupropion is the most evidence‑based, but if you’re anxious about anxiety spikes, start with buspirone or a low‑dose dopaminergic agent.
Patient factors matter: age, gender, relationship status, and comorbidities (e.g., hypertension, anxiety) can tilt the balance. For younger, sexually active adults, a drug holiday might be acceptable. For older patients or those with cardiovascular risk, avoid agents that increase heart rate (e.g., ropinirole).
Practical Tips for Clinicians & Patients
- Open the conversation early. Only 42 % of primary‑care doctors know the best strategies (J. Clin. Psychiatry, 2022). Bring up sexual side effects at the first follow‑up.
- Document every assessment. Use ASEX or the Antidepressant Sexual Dysfunction Inventory at baseline, 4 weeks, and monthly thereafter for the first 3 months.
- Set realistic timelines. Most pharmacologic adjuncts need 2‑4 weeks to show a full effect; drug holidays work within days.
- Combine with behavioral techniques. Sensate‑focus exercises, exploring new fantasies, or using a vibrator can boost arousal while medication adjustments take effect (Reddit user SexTherapistAmy’s report of 50 % improvement).
- Leverage community resources. The Sexual Health Network’s clinician directory (1,200+ specialists) and SSRI Stories support community (15,000+ members) provide real‑world outcome data.
Remember, the goal isn’t just to eliminate side effects but to maintain mood stability. If a patient’s depression worsens after a change, be ready to revert or try a different path.
Key Takeaways
- SSRI sexual dysfunction affects up to 70 % of users and is a leading cause of medication discontinuation.
- Early screening (2‑4 weeks) with a validated scale dramatically improves adherence.
- Start simple: dose reduction or a short drug holiday (if using sertraline, citalopram, etc.).
- If symptoms persist, switch to bupropion or another low‑impact antidepressant.
- Adjuncts-especially daily SR‑bupropion-offer the most robust evidence, but each carries specific side‑effect profiles to consider.
- Combine pharmacologic steps with communication, documentation, and behavioral strategies for the best overall outcome.
How soon after starting an SSRI should I expect sexual side effects?
Most patients notice changes within the first 2‑4 weeks. That’s why a follow‑up at week 2 is recommended.
Can I safely reduce my SSRI dose without worsening depression?
A 25‑50 % reduction often improves sexual function while maintaining efficacy for mild‑to‑moderate depression. Monitor mood closely for at least two weeks after the change.
Are drug holidays effective for all SSRIs?
Only for short‑half‑life agents (sertraline, citalopram, fluvoxamine). Fluoxetine’s long half‑life means a holiday won’t clear the drug from your system quickly enough.
What’s the evidence behind bupropion augmentation?
In a placebo‑controlled trial of 55 patients on various SSRIs, sustained‑release bupropion 150 mg twice daily improved desire and sexual frequency by 66 % (Jing et al., 2016, p=.024).
Should I try a dopaminergic agent like ropinirole?
Ropinirole can work within 48‑72 hours, but about 30 % of users develop anxiety or tremor, especially when combined with fluoxetine. It’s best for patients who can’t tolerate bupropion.



eko lennon on 25 October 2025, AT 17:58 PM
I have spent countless nights scrolling through clinical trials, patient forums, and obscure Reddit threads, trying to piece together a coherent strategy for battling SSRI‑induced sexual dysfunction.
What I discovered is that the journey is not merely a medical adjustment but an odyssey through the labyrinth of one’s own psyche.
First, you must acknowledge the paradox that the very drug rescuing you from the abyss of depression simultaneously clamps the engine of desire.
This acknowledgment, though painful, becomes the cornerstone of any successful intervention.
Second, the timing of your assessments is crucial; a two‑week checkpoint feels like a lifetime when you are desperate for intimacy.
During that window, use validated scales such as ASEX, because anecdotal self‑reporting is as unreliable as guessing the weather by looking at clouds.
Third, when the data confirm a decline, the clinician should not shy away from a calculated dose reduction, even if it feels like flirting with relapse.
Studies show a quarter‑to‑half reduction can restore libido in up to sixty percent of patients while preserving the antidepressant effect.
If that maneuver fails, consider a drug holiday, but only with short‑half‑life agents; otherwise you are merely rearranging the same chemical deck.
The holiday must be carefully timed-48 to 72 hours before intimacy-to avoid withdrawal symptoms that could masquerade as worsening depression.
When holidays are impractical, the next logical step is a switch to bupropion, a dopamine‑noradrenaline reuptake inhibitor that sidesteps serotonergic suppression.
The transition requires a titration period of two to four weeks, during which monitoring for mood destabilization is non‑negotiable.
Adjunctive therapies, such as low‑dose ropinirole or buspirone, can be layered on, yet each carries its own side‑effect profile that must be weighed against the potential gain.
Beyond pharmacology, behavioral techniques like sensate‑focus exercises provide a neuro‑plastic boost that can synergize with medication changes.
In practice, the best outcomes arise from a personalized algorithm: start simple, document rigorously, and only escalate when the evidence demands it.
Remember, the ultimate goal is not just the absence of dysfunction but the restoration of a satisfying, authentic sexual experience that complements your mental health.