Heart Failure Alcohol Risk Calculator
When dealing with Congestive Heart Failure, a chronic condition where the heart cannot pump blood efficiently, adding Alcohol Consumption into the mix can dramatically change the disease trajectory.
Why the Link Matters
Doctors see a clear pattern: patients who drink regularly often experience faster symptom progression, more frequent hospitalizations, and a higher mortality rate. Understanding the biological pathways helps you make smarter choices.
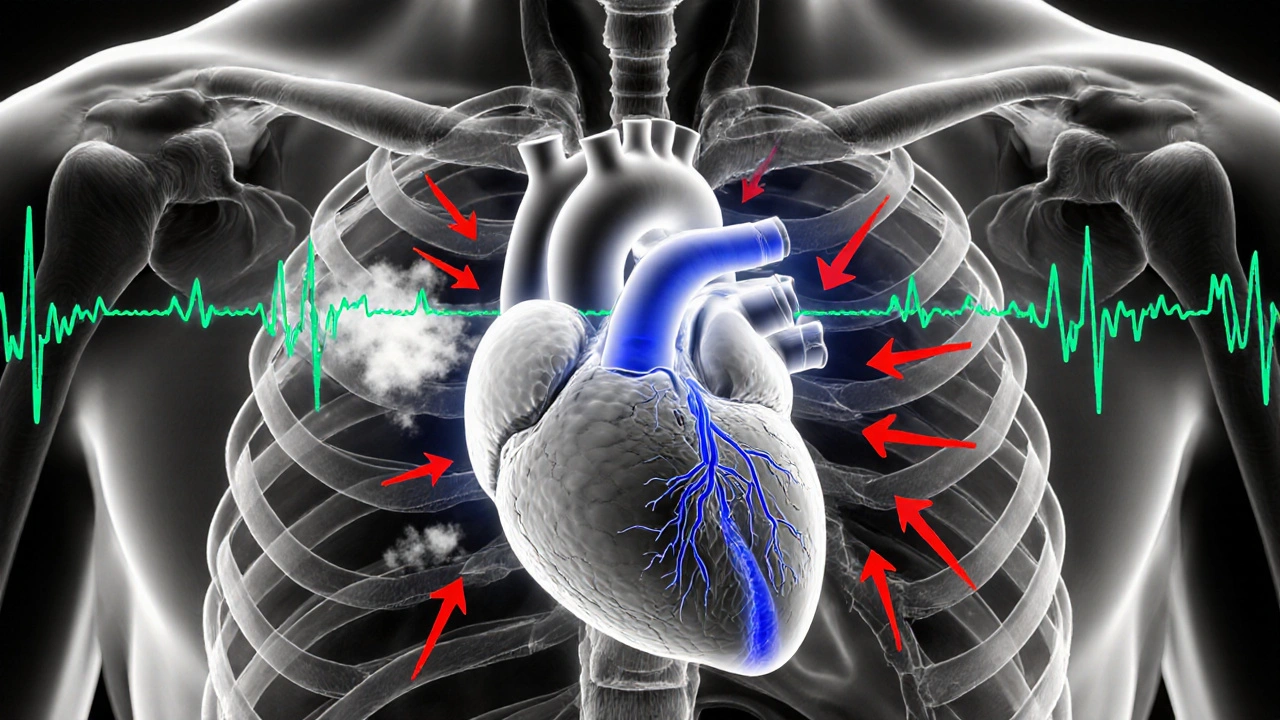
Physiological Effects of Alcohol on a Failing Heart
Alcohol exerts several direct actions that worsen heart function:
- Myocardial toxicity: Even moderate doses can damage heart muscle cells, a condition known as alcoholic cardiomyopathy.
- Fluid retention: Alcohol is a diuretic at first, but chronic use triggers hormonal changes that increase sodium and water re‑absorption, worsening pulmonary edema.
- Blood pressure spikes: Acute intake raises systolic pressure, putting extra strain on an already weakened ventricle.
- Arrhythmia risk: Binge drinking often precipitates atrial fibrillation, which reduces cardiac output and can trigger sudden decompensation.
All these mechanisms feed into the core problem of congestive heart failure: the heart’s inability to meet the body’s oxygen demands.
What the Evidence Says
Large cohort studies from the United States, Europe, and Asia consistently show a dose‑response relationship. One 2023 meta‑analysis of 12 studies (over 350,000 participants) found:
- Low‑level drinkers (≤1 drink per day) had a 7% higher risk of developing CHF compared with abstainers.
- Moderate drinkers (1-2 drinks per day) faced a 15% increase.
- Heavy drinkers (≥3 drinks per day) experienced a 42% jump in risk.
Importantly, the increased risk persisted even after adjusting for common confounders such as smoking, hypertension, and diabetes.
How Much Is Too Much?
| Intake Level | Typical Daily Drinks | Effect on Heart Function | Hospitalization Risk |
|---|---|---|---|
| Low | ≤1 | Minor increase in blood pressure; slight reduction in ejection fraction over years. | Small but measurable rise. |
| Moderate | 1-2 | Noticeable myocardial remodeling; higher incidence of atrial fibrillation. | Significant increase, especially in patients older than 65. |
| High | ≥3 | Alcoholic cardiomyopathy develops; rapid decline in left ventricular ejection fraction. | Very high; frequent readmissions for decompensation. |
Managing Alcohol When You Have CHF
Guidelines from the American Heart Association (2024) recommend total abstinence for patients with advanced stages (NYHA III‑IV). For those in earlier stages, a strict limit of one standard drink per day-if any-is advised.
Practical steps:
- Track every drink in a journal or smartphone app.
- Replace alcoholic beverages with water, herbal tea, or low‑sugar mocktails during meals.
- Discuss any occasional social drinking with your cardiologist; they may adjust diuretic dosing.
- Watch for early warning signs: sudden weight gain (>2kg in 48hours), swelling of ankles, or new shortness of breath.
Medication Interactions You Can’t Ignore
Alcohol can blunt the effectiveness of many CHF drugs:
- Beta‑Blockers: Alcohol raises heart rate, counteracting the slowing effect.
- ACE Inhibitors and ARBs: Combined use may cause dangerous drops in blood pressure.
- Warfarin (if prescribed for atrial fibrillation): Alcohol alters clotting dynamics, increasing bleed risk.
- Diuretics: Dehydration from alcohol can lead to electrolyte imbalances, triggering arrhythmias.
Always tell your prescriber about any drinking habits.
Lifestyle Factors That Compound Alcohol’s Harm
Alcohol doesn’t act in isolation. High sodium intake, sedentary behavior, and uncontrolled hypertension amplify its negative impact.
Combining a low‑sodium diet (≤2g of sodium per day) with regular aerobic activity- even a brisk 30‑minute walk-can offset some of the vascular damage caused by occasional drinks.
Frequently Asked Questions
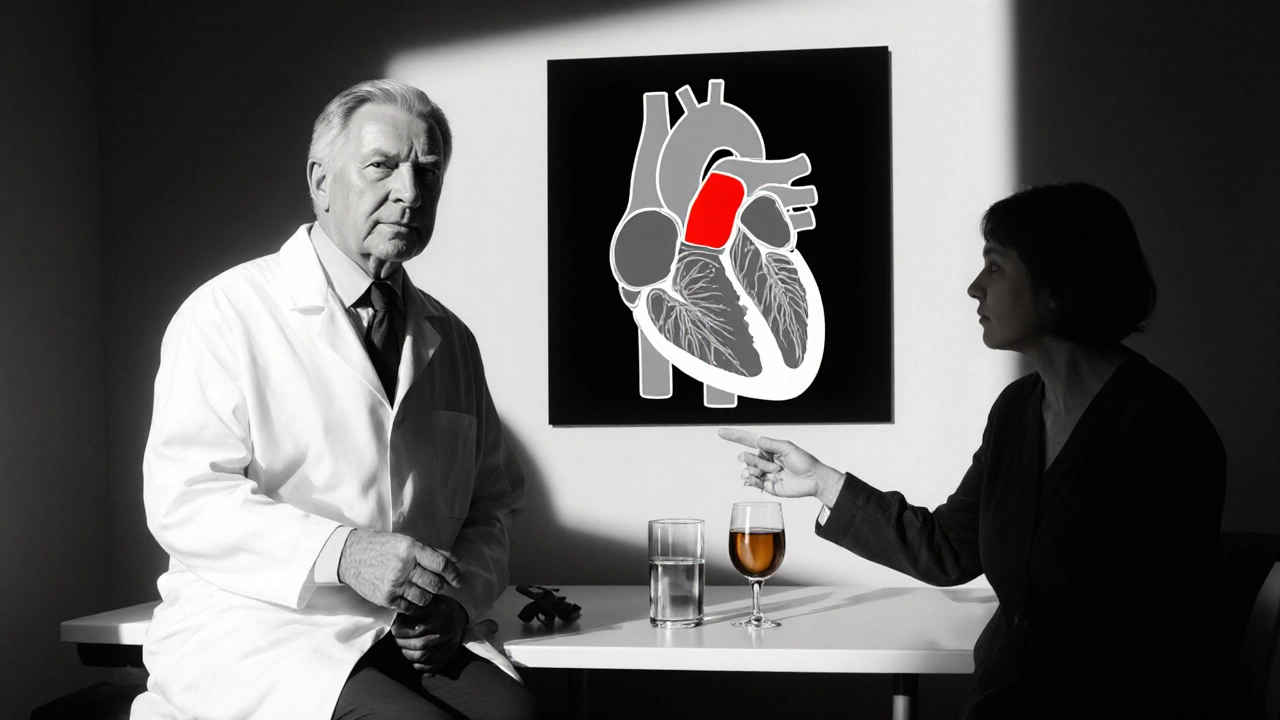
Can a single glass of wine be safe for someone with congestive heart failure?
Most guidelines advise complete abstinence in moderate to severe CHF (NYHA class II‑IV). In early-stage disease, one glass (≈150ml) might be permissible, but only if your doctor has approved it and you monitor weight and symptoms closely.
How quickly can alcohol worsen heart failure symptoms?
Binge drinking can trigger acute decompensation within hours, leading to sudden shortness of breath and rapid weight gain. Regular moderate drinking may take months or years to show measurable decline in ejection fraction.
Does quitting alcohol improve heart function?
Yes. Studies show that patients who stop drinking experience a modest improvement in left ventricular ejection fraction (average 3‑5%) and a reduction in hospital readmissions within the first year.
Are there any safe alcohol‑free alternatives for social situations?
Sparkling water with a splash of citrus, non‑alcoholic craft beers, or herbal mocktails provide the ritual without the risk. Many venues now list zero‑alcohol options on their menus.
What warning signs should prompt an emergency call?
Sudden swelling of the legs or abdomen, sharp chest pain, severe shortness of breath, or fainting spells after drinking should be treated as emergencies.


RJ Samuel on 16 October 2025, AT 20:56 PM
Sure, the article acts like every sip is a death sentence, but honestly the panic’s overblown. A dram of whisky can be a tiny rebellion against a sterile regimen, and it doesn’t magically turn your heart into a sinkhole. Think of it as a splash of color in a gray routine, not a thunderstorm.